HAEM5:ALK-positive anaplastic large cell lymphoma: Difference between revisions
| [unchecked revision] | [checked revision] |
Bailey.Glen (talk | contribs) No edit summary |
Bailey.Glen (talk | contribs) No edit summary |
||
| (9 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{DISPLAYTITLE:ALK-positive anaplastic large cell lymphoma}} | {{DISPLAYTITLE:ALK-positive anaplastic large cell lymphoma}} | ||
[[HAEM5:Table_of_Contents|Haematolymphoid Tumours (WHO Classification, 5th ed.)]] | [[HAEM5:Table_of_Contents|Haematolymphoid Tumours (WHO Classification, 5th ed.)]] | ||
{{Under Construction}} | {{Under Construction}} | ||
<blockquote class= | <blockquote class="blockedit">{{Box-round|title=Content Update To WHO 5th Edition Classification Is In Process; Content Below is Based on WHO 4th Edition Classification|This page was converted to the new template on 2023-12-07. The original page can be found at [[HAEM4:Anaplastic Large Cell Lymphoma, ALK-Positive]]. | ||
}}</blockquote> | }}</blockquote> | ||
| Line 15: | Line 14: | ||
Sumire Kitahara, MD, Cedars-Sinai, Los Angeles, CA | Sumire Kitahara, MD, Cedars-Sinai, Los Angeles, CA | ||
==WHO Classification of Disease== | ==WHO Classification of Disease== | ||
| Line 39: | Line 35: | ||
|ALK-positive anaplastic large cell lymphoma | |ALK-positive anaplastic large cell lymphoma | ||
|} | |} | ||
==Related Terminology== | |||
{| class="wikitable" | {| class="wikitable" | ||
| | |+ | ||
| | |Acceptable | ||
|Anaplastic large cell lymphoma, ALK-positive | |||
|- | |- | ||
| | |Not Recommended | ||
| | |N/A | ||
|} | |} | ||
==Gene Rearrangements== | |||
Put your text here and fill in the table <span style="color:#0070C0">(''Instructions: Details on clinical significance such as prognosis and other important information can be provided in the notes section. Please include references throughout the table. Do not delete the table.'')</span> | |||
Put your text here and fill in the table <span style="color:#0070C0">('' | |||
{| class="wikitable sortable" | {| class="wikitable sortable" | ||
|- | |- | ||
! | !Driver Gene!!Fusion(s) and Common Partner Genes!!Molecular Pathogenesis!!Typical Chromosomal Alteration(s) | ||
!Prevalence -Common >20%, Recurrent 5-20% or Rare <5% (Disease) | |||
!Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | |||
!Established Clinical Significance Per Guidelines - Yes or No (Source) | |||
!Clinical Relevance Details/Other Notes | |||
|- | |- | ||
| | |<span class="blue-text">EXAMPLE:</span> ''ABL1''||<span class="blue-text">EXAMPLE:</span> ''BCR::ABL1''||<span class="blue-text">EXAMPLE:</span> The pathogenic derivative is the der(22) resulting in fusion of 5’ BCR and 3’ABL1.||<span class="blue-text">EXAMPLE:</span> t(9;22)(q34;q11.2) | ||
|<span class="blue-text">EXAMPLE:</span> Common (CML) | |||
|<span class="blue-text">EXAMPLE:</span> D, P, T | |||
|<span class="blue-text">EXAMPLE:</span> Yes (WHO, NCCN) | |||
|<span class="blue-text">EXAMPLE:</span> | |||
The t(9;22) is diagnostic of CML in the appropriate morphology and clinical context (add reference). This fusion is responsive to targeted therapy such as Imatinib (Gleevec) (add reference). BCR::ABL1 is generally favorable in CML (add reference). | |||
|- | |- | ||
| | |<span class="blue-text">EXAMPLE:</span> ''CIC'' | ||
|- | |<span class="blue-text">EXAMPLE:</span> ''CIC::DUX4'' | ||
| | |<span class="blue-text">EXAMPLE:</span> Typically, the last exon of ''CIC'' is fused to ''DUX4''. The fusion breakpoint in ''CIC'' is usually intra-exonic and removes an inhibitory sequence, upregulating ''PEA3'' genes downstream of ''CIC'' including ''ETV1'', ''ETV4'', and ''ETV5''. | ||
|<span class="blue-text">EXAMPLE:</span> t(4;19)(q25;q13) | |||
|<span class="blue-text">EXAMPLE:</span> Common (CIC-rearranged sarcoma) | |||
|- | |<span class="blue-text">EXAMPLE:</span> D | ||
| | | | ||
| | |<span class="blue-text">EXAMPLE:</span> | ||
| | ''DUX4'' has many homologous genes; an alternate translocation in a minority of cases is t(10;19), but this is usually indistinguishable from t(4;19) by short-read sequencing (add references). | ||
| | |||
|- | |- | ||
| | |<span class="blue-text">EXAMPLE:</span> ''ALK'' | ||
|<span class="blue-text">EXAMPLE:</span> ''ELM4::ALK'' | |||
| | |||
< | Other fusion partners include ''KIF5B, NPM1, STRN, TFG, TPM3, CLTC, KLC1'' | ||
|<span class="blue-text">EXAMPLE:</span> Fusions result in constitutive activation of the ''ALK'' tyrosine kinase. The most common ''ALK'' fusion is ''EML4::ALK'', with breakpoints in intron 19 of ''ALK''. At the transcript level, a variable (5’) partner gene is fused to 3’ ''ALK'' at exon 20. Rarely, ''ALK'' fusions contain exon 19 due to breakpoints in intron 18. | |||
|<span class="blue-text">EXAMPLE:</span> N/A | |||
|<span class="blue-text">EXAMPLE:</span> Rare (Lung adenocarcinoma) | |||
|<span class="blue-text">EXAMPLE:</span> T | |||
| | |||
|<span class="blue-text">EXAMPLE:</span> | |||
Both balanced and unbalanced forms are observed by FISH (add references). | |||
|- | |||
|<span class="blue-text">EXAMPLE:</span> ''ABL1'' | |||
|<span class="blue-text">EXAMPLE:</span> N/A | |||
|<span class="blue-text">EXAMPLE:</span> Intragenic deletion of exons 2–7 in ''EGFR'' removes the ligand-binding domain, resulting in a constitutively active tyrosine kinase with downstream activation of multiple oncogenic pathways. | |||
|<span class="blue-text">EXAMPLE:</span> N/A | |||
|<span class="blue-text">EXAMPLE:</span> Recurrent (IDH-wildtype Glioblastoma) | |||
|<span class="blue-text">EXAMPLE:</span> D, P, T | |||
| | |||
< | |||
< | |||
</ | |||
<span | |||
| | |||
| | | | ||
|- | |- | ||
| | | | ||
| | | | ||
| | | | ||
| | | | ||
| | | | ||
| | |||
| | |||
| | | | ||
|} | |} | ||
FISH is not required for diagnosis in routine practice <ref name=":27" /><ref name=":28" />. | FISH is not required for diagnosis in routine practice <ref name=":27" /><ref name=":28" />. | ||
| Line 215: | Line 118: | ||
!Notes | !Notes | ||
|- | |- | ||
|t(2;5)(p23;q35)||3' ''ALK'' / 5' ''NPM1''<ref name=":20" />||''NPM1::ALK'' fusion protein||84%<ref name=":0" /> | |t(2;5)(p23;q35)||3' ''ALK'' / 5' ''NPM1''<ref name=":20" />||''NPM1::ALK'' fusion protein||84%<ref name=":0">Arber DA, et al., (2017). Anaplastic large cell lymphoma, ALK-positive, in World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues, Revised 4th edition. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Arber DA, Hasserjian RP, Le Beau MM, Orazi A, and Siebert R, Editors. IARC Press: Lyon, France, p413-418.</ref> | ||
|No | |No | ||
|No | |No | ||
| Line 222: | Line 125: | ||
<u>Of note, identifying the ''ALK'' fusion partner is not considered necessary in routine clinical practice.</u> | |||
| Line 318: | Line 221: | ||
<blockquote class= | <blockquote class="blockedit">{{Box-round|title=v4:Chromosomal Rearrangements (Gene Fusions)|The content below was from the old template. Please incorporate above.}}</blockquote> | ||
*ALK(+) ALCL is characterized by chromosomal translocations involving ''ALK'' gene, a receptor tyrosine kinase domain at 2p23. | *ALK(+) ALCL is characterized by chromosomal translocations involving ''ALK'' gene, a receptor tyrosine kinase domain at 2p23. | ||
| Line 387: | Line 290: | ||
<blockquote class= | <blockquote class="blockedit">{{Box-round|title=v4:Clinical Significance (Diagnosis, Prognosis and Therapeutic Implications).|Please incorporate this section into the relevant tables found in: | ||
* Chromosomal Rearrangements (Gene Fusions) | * Chromosomal Rearrangements (Gene Fusions) | ||
* Individual Region Genomic Gain/Loss/LOH | * Individual Region Genomic Gain/Loss/LOH | ||
| Line 425: | Line 328: | ||
---- | ---- | ||
</blockquote> | </blockquote> | ||
==Individual Region Genomic Gain/Loss/LOH== | ==Individual Region Genomic Gain/Loss/LOH== | ||
Put your text here and fill in the table <span style="color:#0070C0">(''Instructions: Includes aberrations not involving gene rearrangements. Details on clinical significance such as prognosis and other important information can be provided in the notes section. Can refer to CGC workgroup tables as linked on the homepage if applicable. Please include references throughout the table. Do not delete the table.'') </span> | |||
Put your text here and fill in the table <span style="color:#0070C0">(''Instructions: Includes aberrations not involving gene | {| class="wikitable sortable" | ||
|- | |||
!Chr #!!Gain, Loss, Amp, LOH!!Minimal Region Cytoband and/or Genomic Coordinates [Genome Build; Size]!!Relevant Gene(s) | |||
!Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | |||
!Established Clinical Significance Per Guidelines - Yes or No (Source) | |||
!Clinical Relevance Details/Other Notes | |||
|- | |||
|<span class="blue-text">EXAMPLE:</span> | |||
7 | |||
|<span class="blue-text">EXAMPLE:</span> Loss | |||
|<span class="blue-text">EXAMPLE:</span> | |||
chr7 | |||
|<span class="blue-text">EXAMPLE:</span> | |||
Unknown | |||
|<span class="blue-text">EXAMPLE:</span> D, P | |||
|<span class="blue-text">EXAMPLE:</span> No | |||
|<span class="blue-text">EXAMPLE:</span> | |||
Presence of monosomy 7 (or 7q deletion) is sufficient for a diagnosis of AML with MDS-related changes when there is ≥20% blasts and no prior therapy (add reference). Monosomy 7/7q deletion is associated with a poor prognosis in AML (add references). | |||
|- | |||
|<span class="blue-text">EXAMPLE:</span> | |||
8 | |||
|<span class="blue-text">EXAMPLE:</span> Gain | |||
|<span class="blue-text">EXAMPLE:</span> | |||
chr8 | |||
|<span class="blue-text">EXAMPLE:</span> | |||
Unknown | |||
|<span class="blue-text">EXAMPLE:</span> D, P | |||
| | |||
|<span class="blue-text">EXAMPLE:</span> | |||
Common recurrent secondary finding for t(8;21) (add references). | |||
|- | |||
|<span class="blue-text">EXAMPLE:</span> | |||
17 | |||
|<span class="blue-text">EXAMPLE:</span> Amp | |||
|<span class="blue-text">EXAMPLE:</span> | |||
17q12; chr17:39,700,064-39,728,658 [hg38; 28.6 kb] | |||
|<span class="blue-text">EXAMPLE:</span> | |||
''ERBB2'' | |||
|<span class="blue-text">EXAMPLE:</span> D, P, T | |||
| | |||
|<span class="blue-text">EXAMPLE:</span> | |||
Amplification of ''ERBB2'' is associated with HER2 overexpression in HER2 positive breast cancer (add references). Add criteria for how amplification is defined. | |||
|- | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|} | |||
{| class="wikitable sortable" | {| class="wikitable sortable" | ||
| Line 474: | Line 428: | ||
|} | |} | ||
<blockquote class= | <blockquote class="blockedit">{{Box-round|title=v4:Genomic Gain/Loss/LOH|The content below was from the old template. Please incorporate above.}}</blockquote> | ||
Frequent secondary chromosomal imbalances are seen in ALK+ ALCL (58% of cases), as based on comparative genomic hybridization analysis<ref>{{Cite journal|last=I|first=Salaverria|last2=S|first2=Beà|last3=A|first3=Lopez-Guillermo|last4=V|first4=Lespinet|last5=M|first5=Pinyol|last6=B|first6=Burkhardt|last7=L|first7=Lamant|last8=A|first8=Zettl|last9=D|first9=Horsman|date=2008|title=Genomic profiling reveals different genetic aberrations in systemic ALK-positive and ALK-negative anaplastic large cell lymphomas|url=https://pubmed.ncbi.nlm.nih.gov/18275429/|language=en|pmid=18275429}}</ref>. | Frequent secondary chromosomal imbalances are seen in ALK+ ALCL (58% of cases), as based on comparative genomic hybridization analysis<ref>{{Cite journal|last=I|first=Salaverria|last2=S|first2=Beà|last3=A|first3=Lopez-Guillermo|last4=V|first4=Lespinet|last5=M|first5=Pinyol|last6=B|first6=Burkhardt|last7=L|first7=Lamant|last8=A|first8=Zettl|last9=D|first9=Horsman|date=2008|title=Genomic profiling reveals different genetic aberrations in systemic ALK-positive and ALK-negative anaplastic large cell lymphomas|url=https://pubmed.ncbi.nlm.nih.gov/18275429/|language=en|pmid=18275429}}</ref>. | ||
| Line 527: | Line 481: | ||
---- | ---- | ||
</blockquote> | </blockquote> | ||
==Characteristic Chromosomal or Other Global Mutational Patterns== | ==Characteristic Chromosomal or Other Global Mutational Patterns== | ||
| Line 535: | Line 490: | ||
!Chromosomal Pattern | !Chromosomal Pattern | ||
!Molecular Pathogenesis | !Molecular Pathogenesis | ||
! | !Prevalence - | ||
Common >20%, Recurrent 5-20% or Rare <5% (Disease) | |||
! | !Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | ||
! | !Established Clinical Significance Per Guidelines - Yes or No (Source) | ||
! | !Clinical Relevance Details/Other Notes | ||
|- | |- | ||
|<span class="blue-text">EXAMPLE:</span> | |<span class="blue-text">EXAMPLE:</span> | ||
| Line 565: | Line 520: | ||
|} | |} | ||
<blockquote class= | <blockquote class="blockedit">{{Box-round|title=v4:Characteristic Chromosomal Aberrations / Patterns|The content below was from the old template. Please incorporate above.}}</blockquote> | ||
See other sections. | See other sections. | ||
| Line 574: | Line 529: | ||
</blockquote> | </blockquote> | ||
==Gene Mutations (SNV/INDEL)== | ==Gene Mutations (SNV/INDEL)== | ||
{| class="wikitable sortable" | |||
|- | |||
!Gene!!Genetic Alteration!!Tumor Suppressor Gene, Oncogene, Other!!Prevalence - | |||
Common >20%, Recurrent 5-20% or Rare <5% (Disease) | |||
!Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | |||
!Established Clinical Significance Per Guidelines - Yes or No (Source) | |||
!Clinical Relevance Details/Other Notes | |||
|- | |||
|<span class="blue-text">EXAMPLE:</span>''EGFR'' | |||
<br /> | |||
|<span class="blue-text">EXAMPLE:</span> Exon 18-21 activating mutations | |||
|<span class="blue-text">EXAMPLE:</span> Oncogene | |||
|<span class="blue-text">EXAMPLE:</span> Common (lung cancer) | |||
|<span class="blue-text">EXAMPLE:</span> T | |||
|<span class="blue-text">EXAMPLE:</span> Yes (NCCN) | |||
|<span class="blue-text">EXAMPLE:</span> Exons 18, 19, and 21 mutations are targetable for therapy. Exon 20 T790M variants cause resistance to first generation TKI therapy and are targetable by second and third generation TKIs (add references). | |||
|- | |||
|<span class="blue-text">EXAMPLE:</span> ''TP53''; Variable LOF mutations | |||
<br /> | |||
|<span class="blue-text">EXAMPLE:</span> Variable LOF mutations | |||
|<span class="blue-text">EXAMPLE:</span> Tumor Supressor Gene | |||
|<span class="blue-text">EXAMPLE:</span> Common (breast cancer) | |||
|<span class="blue-text">EXAMPLE:</span> P | |||
| | |||
|<span class="blue-text">EXAMPLE:</span> >90% are somatic; rare germline alterations associated with Li-Fraumeni syndrome (add reference). Denotes a poor prognosis in breast cancer. | |||
|- | |||
|<span class="blue-text">EXAMPLE:</span> ''BRAF''; Activating mutations | |||
|<span class="blue-text">EXAMPLE:</span> Activating mutations | |||
|<span class="blue-text">EXAMPLE:</span> Oncogene | |||
|<span class="blue-text">EXAMPLE:</span> Common (melanoma) | |||
|<span class="blue-text">EXAMPLE:</span> T | |||
| | |||
| | |||
|- | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|}Note: A more extensive list of mutations can be found in [https://www.cbioportal.org/ <u>cBioportal</u>], [https://cancer.sanger.ac.uk/cosmic <u>COSMIC</u>], and/or other databases. When applicable, gene-specific pages within the CCGA site directly link to pertinent external content. | |||
{| class="wikitable sortable" | {| class="wikitable sortable" | ||
|- | |- | ||
!Gene; Genetic Alteration!! | !Gene; Genetic Alteration!!Presumed Mechanism (Tumor Suppressor Gene [TSG] / Oncogene / Other)!!Prevalence (COSMIC / TCGA / Other)!!Concomitant Mutations!!Mutually Exclusive Mutations | ||
! | !Diagnostic Significance (Yes, No or Unknown) | ||
!Prognostic Significance (Yes, No or Unknown) | !Prognostic Significance (Yes, No or Unknown) | ||
!Therapeutic Significance (Yes, No or Unknown) | !Therapeutic Significance (Yes, No or Unknown) | ||
| Line 631: | Line 628: | ||
<blockquote class= | <blockquote class="blockedit">{{Box-round|title=v4:Gene Mutations (SNV/INDEL)|The content below was from the old template. Please incorporate above.}}</blockquote> | ||
*Limited literature on somatic mutations in ALK+ ALCL | *Limited literature on somatic mutations in ALK+ ALCL | ||
| Line 682: | Line 679: | ||
---- | ---- | ||
</blockquote> | </blockquote> | ||
==Epigenomic Alterations== | ==Epigenomic Alterations== | ||
| Line 715: | Line 713: | ||
|} | |} | ||
<blockquote class= | <blockquote class="blockedit"> | ||
*ALK-NPM-STAT3 induces: | *ALK-NPM-STAT3 induces: | ||
**See Epigenomics section above | **See Epigenomics section above | ||
| Line 726: | Line 724: | ||
</blockquote> | </blockquote> | ||
<blockquote class= | <blockquote class="blockedit">{{Box-round|title=v4:Genes and Main Pathways Involved|The content below was from the old template. Please incorporate above.}}</blockquote> | ||
* | * | ||
| Line 758: | Line 756: | ||
==Additional Information== | ==Additional Information== | ||
This disease is <u>defined/characterized</u> as detailed below: | |||
Anaplastic Large Cell Lymphoma, ALK-Positive (ALK+ ALCL) is a T-cell lymphoma characterized by usually large lymphoma cells with abundant cytoplasm and pleomorphic nuclei, often horse-shoe shaped (see Morphologic Features below), with a chromosomal rearrangement involving the ALK gene resulting in expression of ALK protein and CD30 | |||
* | The <u>epidemiology/prevalence</u> of this disease is detailed below: | ||
*ALCL ([[ALK]]+, ALK-, and primary cutaneous) account for <5% of all cases of non-Hodgkin lymphoma (NHL)<ref name=":0" /> | |||
*ALK+ ALCL<ref name=":0" /> | |||
**~3% of adult NHL | |||
**10-20% of childhood lymphomas | |||
**Most frequent in the first three decades of life | |||
**Male:female = 1.5:1 | |||
The <u>clinical features</u> of this disease are detailed below: | |||
Signs and symptoms - Most patients (70%) present with advanced (stage III-IV) disease and B-symptoms.<ref name=":19">{{Cite journal|last=Savage|first=Kerry J.|last2=Harris|first2=Nancy Lee|last3=Vose|first3=Julie M.|last4=Ullrich|first4=Fred|last5=Jaffe|first5=Elaine S.|last6=Connors|first6=Joseph M.|last7=Rimsza|first7=Lisa|last8=Pileri|first8=Stefano A.|last9=Chhanabhai|first9=Mukesh|date=2008-06-15|title=ALK- anaplastic large-cell lymphoma is clinically and immunophenotypically different from both ALK+ ALCL and peripheral T-cell lymphoma, not otherwise specified: report from the International Peripheral T-Cell Lymphoma Project|url=https://pubmed.ncbi.nlm.nih.gov/18385450/|journal=Blood|volume=111|issue=12|pages=5496–5504|doi=10.1182/blood-2008-01-134270|issn=1528-0020|pmid=18385450}}</ref> | |||
Laboratory findings - Noncontributory | |||
The <u>sites of involvement</u> of this disease are detailed below: | |||
*Lymph nodes and extranodal sites (most commonly skin, bone, soft tissue, lungs and liver)<ref name=":0" /> | |||
*Bone marrow involvement detected in 30% when using immunohistochemistry (CD30 and EMA). Can miss marrow involvement by H&E evaluation alone, which detects involvement with ~10% incidence.<ref>{{Cite journal|last=M|first=Fraga|last2=P|first2=Brousset|last3=D|first3=Schlaifer|last4=C|first4=Payen|last5=A|first5=Robert|last6=H|first6=Rubie|last7=F|first7=Huguet-Rigal|last8=G|first8=Delsol|date=1995|title=Bone marrow involvement in anaplastic large cell lymphoma. Immunohistochemical detection of minimal disease and its prognostic significance|url=https://pubmed.ncbi.nlm.nih.gov/7817951/|language=en|pmid=7817951}}</ref> | |||
The <u>morphologic features</u> of this disease are detailed below: | |||
"Hallmark cells"<ref>{{Cite journal|last=Stein|first=H.|last2=Foss|first2=H. D.|last3=Dürkop|first3=H.|last4=Marafioti|first4=T.|last5=Delsol|first5=G.|last6=Pulford|first6=K.|last7=Pileri|first7=S.|last8=Falini|first8=B.|date=2000-12-01|title=CD30(+) anaplastic large cell lymphoma: a review of its histopathologic, genetic, and clinical features|url=https://pubmed.ncbi.nlm.nih.gov/11090048/|journal=Blood|volume=96|issue=12|pages=3681–3695|issn=0006-4971|pmid=11090048}}</ref><ref>{{Cite journal|last=Benharroch|first=D.|last2=Meguerian-Bedoyan|first2=Z.|last3=Lamant|first3=L.|last4=Amin|first4=C.|last5=Brugières|first5=L.|last6=Terrier-Lacombe|first6=M. J.|last7=Haralambieva|first7=E.|last8=Pulford|first8=K.|last9=Pileri|first9=S.|date=1998-03-15|title=ALK-positive lymphoma: a single disease with a broad spectrum of morphology|url=https://pubmed.ncbi.nlm.nih.gov/9490693/|journal=Blood|volume=91|issue=6|pages=2076–2084|issn=0006-4971|pmid=9490693}}</ref> | |||
*Lymphoma cells characterized by eccentric, horseshoe-shaped or kidney-shaped nuclei, often with eosinophilic cytoplasm accentuated near the nucleus | |||
*Usually large in size, but may also be smaller | |||
*Present in varying proportions | |||
*Seen in all morphological variants/patterns of ALK+ ALCL | |||
Morphological variants/patterns | |||
#Common (60%): predominant population of large hallmark cells | |||
#Lymphohistiocytic (10%): lymphoma cells are admixed with numerous reactive histiocytes that may obscure the lymphoma cells; lymphoma cells often cluster around vessels and are often smaller than in the common pattern | |||
#Small cell (5-10%): predominant population of smaller lymphoma cells; hallmark cells are often concentrated around vessels; may also see "fried egg cells" (pale cytoplasm with central nucleus) or signet ring-like cells; can misdiagnose of peripheral T-cell lymphoma, NOS | |||
#Hodgkin-like (3%): mimics nodular sclerosis classic Hodgkin lymphoma | |||
#Composite (15%): more than one pattern in a single lymph node | |||
When lymph node is only partially involved, lymphoma characteristically grows in the sinuses, which may mimic a metastatic tumor. | |||
The <u>immunophenotype</u> of this disease is detailed below: | |||
* CD30 expression on ALCL (ALK+ or ALK-) allows for targeted therapy<ref name=":2" />. First-line therapy: [https://www.fda.gov/drugs/fda-approves-brentuximab-vedotin-previously-untreated-salcl-and-cd30-expressing-ptcl Brentuximab] (anti-CD30) vedotin + CHP (cyclophosphamide, doxorubicin, and prednisone) | |||
CD30+''':''' Positive (universal) - cell membrane and Golgi; large lymphoma cells show strongest staining; smaller cells may show weak, partial to negative staining | |||
ALK: Positive (universal) - cellular location of ALK staining varies depending on ALK translocation partner. In the most common t(2;5), most cases show both cytoplasmic and nuclear | |||
EMA: positive (subset) | |||
CD3: Positive (subset) | |||
CD4: Positive (70%) | |||
CD5: Negative in majority of cases | |||
CD8: Positive in majority of cases | |||
CD2: Positive in majority of cases | |||
TIA1: Positive | |||
Granzyme B: Positive | |||
Perforin: Positive | |||
CD45: Variably positive | |||
CD25: Positive (universal) | |||
BCL2: Negative (universal) | |||
==Links== | ==Links== | ||
| Line 778: | Line 849: | ||
<nowiki>*</nowiki>''Citation of this Page'': “ALK-positive anaplastic large cell lymphoma”. Compendium of Cancer Genome Aberrations (CCGA), Cancer Genomics Consortium (CGC), updated {{REVISIONMONTH}}/{{REVISIONDAY}}/{{REVISIONYEAR}}, <nowiki>https://ccga.io/index.php/HAEM5:ALK-positive_anaplastic_large_cell_lymphoma</nowiki>. | <nowiki>*</nowiki>''Citation of this Page'': “ALK-positive anaplastic large cell lymphoma”. Compendium of Cancer Genome Aberrations (CCGA), Cancer Genomics Consortium (CGC), updated {{REVISIONMONTH}}/{{REVISIONDAY}}/{{REVISIONYEAR}}, <nowiki>https://ccga.io/index.php/HAEM5:ALK-positive_anaplastic_large_cell_lymphoma</nowiki>. | ||
Latest revision as of 10:30, 4 September 2025
Haematolymphoid Tumours (WHO Classification, 5th ed.)
| This page is under construction |
editContent Update To WHO 5th Edition Classification Is In Process; Content Below is Based on WHO 4th Edition ClassificationThis page was converted to the new template on 2023-12-07. The original page can be found at HAEM4:Anaplastic Large Cell Lymphoma, ALK-Positive.
(General Instructions – The focus of these pages is the clinically significant genetic alterations in each disease type. This is based on up-to-date knowledge from multiple resources such as PubMed and the WHO classification books. The CCGA is meant to be a supplemental resource to the WHO classification books; the CCGA captures in a continually updated wiki-stye manner the current genetics/genomics knowledge of each disease, which evolves more rapidly than books can be revised and published. If the same disease is described in multiple WHO classification books, the genetics-related information for that disease will be consolidated into a single main page that has this template (other pages would only contain a link to this main page). Use HUGO-approved gene names and symbols (italicized when appropriate), HGVS-based nomenclature for variants, as well as generic names of drugs and testing platforms or assays if applicable. Please complete tables whenever possible and do not delete them (add N/A if not applicable in the table and delete the examples); to add (or move) a row or column in a table, click nearby within the table and select the > symbol that appears. Please do not delete or alter the section headings. The use of bullet points alongside short blocks of text rather than only large paragraphs is encouraged. Additional instructions below in italicized blue text should not be included in the final page content. Please also see Author_Instructions and FAQs as well as contact your Associate Editor or Technical Support.)
Primary Author(s)*
Miguel Gonzalez Mancera, MD, Cedars-Sinai, Los Angeles, CA
Sumire Kitahara, MD, Cedars-Sinai, Los Angeles, CA
WHO Classification of Disease
| Structure | Disease |
|---|---|
| Book | Haematolymphoid Tumours (5th ed.) |
| Category | T-cell and NK-cell lymphoid proliferations and lymphomas |
| Family | Mature T-cell and NK-cell neoplasms |
| Type | Anaplastic large cell lymphoma |
| Subtype(s) | ALK-positive anaplastic large cell lymphoma |
Related Terminology
| Acceptable | Anaplastic large cell lymphoma, ALK-positive |
| Not Recommended | N/A |
Gene Rearrangements
Put your text here and fill in the table (Instructions: Details on clinical significance such as prognosis and other important information can be provided in the notes section. Please include references throughout the table. Do not delete the table.)
| Driver Gene | Fusion(s) and Common Partner Genes | Molecular Pathogenesis | Typical Chromosomal Alteration(s) | Prevalence -Common >20%, Recurrent 5-20% or Rare <5% (Disease) | Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | Established Clinical Significance Per Guidelines - Yes or No (Source) | Clinical Relevance Details/Other Notes |
|---|---|---|---|---|---|---|---|
| EXAMPLE: ABL1 | EXAMPLE: BCR::ABL1 | EXAMPLE: The pathogenic derivative is the der(22) resulting in fusion of 5’ BCR and 3’ABL1. | EXAMPLE: t(9;22)(q34;q11.2) | EXAMPLE: Common (CML) | EXAMPLE: D, P, T | EXAMPLE: Yes (WHO, NCCN) | EXAMPLE:
The t(9;22) is diagnostic of CML in the appropriate morphology and clinical context (add reference). This fusion is responsive to targeted therapy such as Imatinib (Gleevec) (add reference). BCR::ABL1 is generally favorable in CML (add reference). |
| EXAMPLE: CIC | EXAMPLE: CIC::DUX4 | EXAMPLE: Typically, the last exon of CIC is fused to DUX4. The fusion breakpoint in CIC is usually intra-exonic and removes an inhibitory sequence, upregulating PEA3 genes downstream of CIC including ETV1, ETV4, and ETV5. | EXAMPLE: t(4;19)(q25;q13) | EXAMPLE: Common (CIC-rearranged sarcoma) | EXAMPLE: D | EXAMPLE:
DUX4 has many homologous genes; an alternate translocation in a minority of cases is t(10;19), but this is usually indistinguishable from t(4;19) by short-read sequencing (add references). | |
| EXAMPLE: ALK | EXAMPLE: ELM4::ALK
|
EXAMPLE: Fusions result in constitutive activation of the ALK tyrosine kinase. The most common ALK fusion is EML4::ALK, with breakpoints in intron 19 of ALK. At the transcript level, a variable (5’) partner gene is fused to 3’ ALK at exon 20. Rarely, ALK fusions contain exon 19 due to breakpoints in intron 18. | EXAMPLE: N/A | EXAMPLE: Rare (Lung adenocarcinoma) | EXAMPLE: T | EXAMPLE:
Both balanced and unbalanced forms are observed by FISH (add references). | |
| EXAMPLE: ABL1 | EXAMPLE: N/A | EXAMPLE: Intragenic deletion of exons 2–7 in EGFR removes the ligand-binding domain, resulting in a constitutively active tyrosine kinase with downstream activation of multiple oncogenic pathways. | EXAMPLE: N/A | EXAMPLE: Recurrent (IDH-wildtype Glioblastoma) | EXAMPLE: D, P, T | ||
FISH is not required for diagnosis in routine practice [1][2].
| Chromosomal Rearrangement | Genes in Fusion (5’ or 3’ Segments) | Pathogenic Derivative | Prevalence | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|---|---|---|
| t(2;5)(p23;q35) | 3' ALK / 5' NPM1[3] | NPM1::ALK fusion protein | 84%[4] | No | No | Yes | Approximately 80% of cases show a cytogenetic translocation t(2;5) (NPM1-ALK, t(2;5)(p23;q35)) which fuses the ALK gene to the nucleophosmine (NPM) gene at 5q35, resulting in the overexpression and constitutive activation of a chimeric ALK fusion protein, which plays an important role in ALK-mediated oncogenesis.
|
| t(1;2)(q25;p23)[10] | 3' ALK / 5' TPM3 | TPM3::ALK Fusion protein | 13%[10] | No | No | No | |
| inv(2)(p23q35)[11] | 3' ALK / 5' ATIC | ATIC::ALK fusion protein | 1% [11] | No | No | No | |
| t(2;3)(p23;q12.2)[12] | 3' ALK / 5' TFG | TFG::ALK fusion protein | <1% | No | No | No | |
| t(2;17)(p23;q23)[13] | 3' ALK / 5' CLTC | CLTC::ALK fusion protein | <1% | No | No | No | |
| t(X;2)(q11-22;p23)[14] | 3' ALK / 5' MSN | MSN::ALK fusion protein | <1% | No | No | No | |
| t(2;19)(p23;p13.1)[15] | 3' ALK / 5' TPM4 | TPM4::ALK fusion protein | <1% | No | No | No | |
| t(2;22)(p23;q11.2)[16] | 3' ALK / 5' MYH9 | MYH9::ALK fusion protein | <1% | No | No | No | |
| t(2;17)(p23;q25)[15] | 3' ALK / 5' RNF213 | RNF213::ALK fusion protein | <1% | No | No | No | |
| t(2;9)(p23;q33)[17] | 3' ALK / 5' TRAF-1 | TRAF-1::ALK fusion protein | <1% | No | No | No |
editv4:Chromosomal Rearrangements (Gene Fusions)The content below was from the old template. Please incorporate above.
- ALK(+) ALCL is characterized by chromosomal translocations involving ALK gene, a receptor tyrosine kinase domain at 2p23.
- Approximately 80% of cases show a cytogenetic translocation t(2;5) (NPM1-ALK, t(2;5)(p23;q35)) which fuses the ALK gene to the nucleophosmine (NPM) gene at 5q35, resulting in the overexpression and constitutive activation of a chimeric ALK fusion protein, which plays an important role in ALK-mediated oncogenesis.[3]
- ALK translocations may be seen in multiple malignancies including epithelial malignancies[18][19][20][21][22][23], inflammatory myofibroblastic tumor[24][25][26], non-Hodgkin's lymphoma[27][28][29], and ALK+ histiocytosis [30][31][32].
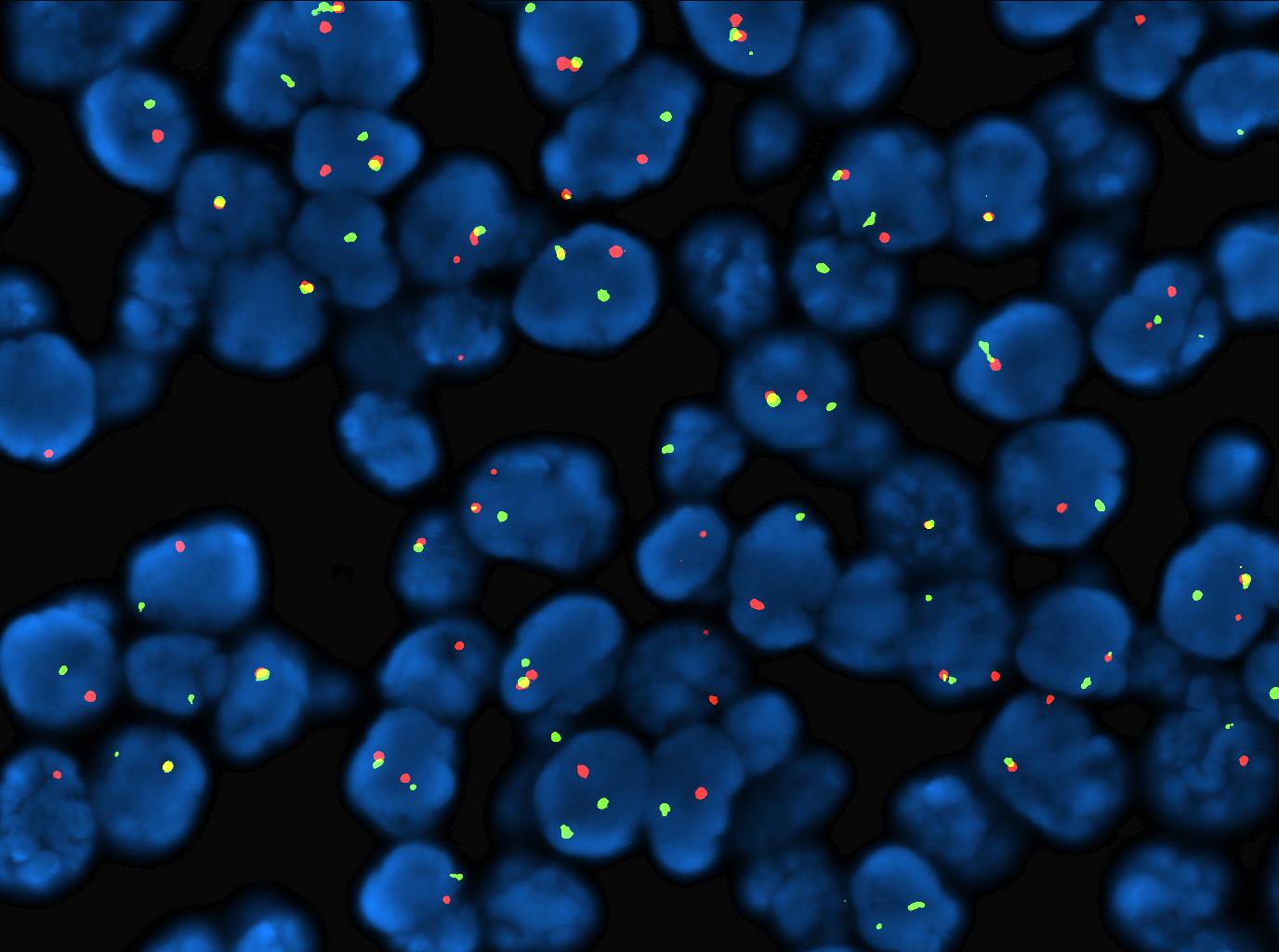
Table below shows described ALK translocations with ALK staining pattern, and frequency of cases. Of note, identifying the ALK fusion partner is not considered necessary in routine clinical practice.
| Chromosomal
Anomaly |
ALK partner | ALK staining pattern | Percentage
of cases |
|---|---|---|---|
| t(2;5)(p23;q35) | NPM1 | Nuclear, nucleolar, diffuse cytoplasmic | 84% |
| t(1;2)(q25;p23)[10] | TPM3 | Diffuse cytoplasmic with peripheral intensification | 13% |
| inv(2)(p23q35)[11] | ATIC | Diffuse cytoplasmic | 1% |
| t(2;3)(p23;q12.2)[12] | TFG | Diffuse cytoplasmic | <1% |
| t(2;17)(p23;q23)[13] | CLTC | Granular cytoplasmic | <1% |
| t(X;2)(q11-22;p23)[14] | MSN | Membrane | <1% |
| t(2;19)(p23;p13.1)[15] | TPM4 | Diffuse cytoplasmic | <1% |
| t(2;22)(p23;q11.2)[16] | MYH9 | Diffuse cytoplasmic | <1% |
| t(2;17)(p23;q25)[15] | RNF213 | Diffuse cytoplasmic | <1% |
| t(2;9)(p23;q33)[17] | TRAF-1 | Diffuse cytoplasmic | <1% |
End of V4 Section
editv4:Clinical Significance (Diagnosis, Prognosis and Therapeutic Implications).Please incorporate this section into the relevant tables found in:
- Chromosomal Rearrangements (Gene Fusions)
- Individual Region Genomic Gain/Loss/LOH
- Characteristic Chromosomal Patterns
- Gene Mutations (SNV/INDEL)
Diagnosis
- As stated above, the diagnosis is based on histology and immunohistochemistry
- FISH is not required for diagnosis in routine practice [1][2]
Prognosis
- ALK+ ALCL has a better survival rate compared to ALK-negative ALCL
- However, differences in patient age (younger in ALK+) may account for this better survival[33]
- Different ALK translocation partners do not have prognostic significance
- Survival is predicted by International Prognostic Index (IPI) with overall long term survival rate approaching 80%
- Detecting minimal residual disease by PCR for NPM1-ALK (not readily commercially available) in bone marrow and peripheral blood during treatment could identify patients at risk of relapse[5]
- Small-cell or lymphohistiocytic patterns tend to present with disseminated disease and have a less favorable prognosis than the common pattern[34]
- NOTCH1 may be a biomarker for risk of relapse[35]
Therapy
- CD30 expression on ALCL (ALK+ or ALK-) allows for targeted therapy[7]
- First-line therapy: Brentuximab (anti-CD30) vedotin + CHP (cyclophosphamide, doxorubicin, and prednisone)
- ALK inhibition (crizotinib) can be an effective 2nd-line therapeutic strategy as ALK is essential for the proliferation and survival of ALK+ ALCL cells[6][7][8]
- Drug resistance may develop due to:
- Mutations of the ALK gene impairing binding of the inhibitor[9]; other ALK inhibitors are not currently FDA-approved for use in ALK+ ALCL
- See also gene mutations section above
- Engagement of other cell signaling pathways
- Drug resistance may develop due to:
- Preclinical models suggest role of:
- Combination therapy with hypomethylating agents (such as azacitidine) and epigenetic modifying drugs (such as romidepsin, a histone deacetylase inhibitor)[36]
- Inhibitors of HSP90 and mTOR inhibition[9]
- NOTCH1 inhibition by γ-secretase inhibitors (GSI) in combination with crizotinib may provide synergistic anti-tumor activity, or as a single agent in ALK-inhibitor resistant cell lines[35]
End of V4 Section
Individual Region Genomic Gain/Loss/LOH
Put your text here and fill in the table (Instructions: Includes aberrations not involving gene rearrangements. Details on clinical significance such as prognosis and other important information can be provided in the notes section. Can refer to CGC workgroup tables as linked on the homepage if applicable. Please include references throughout the table. Do not delete the table.)
| Chr # | Gain, Loss, Amp, LOH | Minimal Region Cytoband and/or Genomic Coordinates [Genome Build; Size] | Relevant Gene(s) | Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | Established Clinical Significance Per Guidelines - Yes or No (Source) | Clinical Relevance Details/Other Notes |
|---|---|---|---|---|---|---|
| EXAMPLE:
7 |
EXAMPLE: Loss | EXAMPLE:
chr7 |
EXAMPLE:
Unknown |
EXAMPLE: D, P | EXAMPLE: No | EXAMPLE:
Presence of monosomy 7 (or 7q deletion) is sufficient for a diagnosis of AML with MDS-related changes when there is ≥20% blasts and no prior therapy (add reference). Monosomy 7/7q deletion is associated with a poor prognosis in AML (add references). |
| EXAMPLE:
8 |
EXAMPLE: Gain | EXAMPLE:
chr8 |
EXAMPLE:
Unknown |
EXAMPLE: D, P | EXAMPLE:
Common recurrent secondary finding for t(8;21) (add references). | |
| EXAMPLE:
17 |
EXAMPLE: Amp | EXAMPLE:
17q12; chr17:39,700,064-39,728,658 [hg38; 28.6 kb] |
EXAMPLE:
ERBB2 |
EXAMPLE: D, P, T | EXAMPLE:
Amplification of ERBB2 is associated with HER2 overexpression in HER2 positive breast cancer (add references). Add criteria for how amplification is defined. | |
| Chr # | Gain / Loss / Amp / LOH | Minimal Region Genomic Coordinates [Genome Build] | Minimal Region Cytoband | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|---|---|---|
| 17p | Gain | 17p11-pter | No | Unclear | No | ||
| 17p | Gain | 17q24 -qter | No | Unclear | No | ||
| 4q | Loss | 4q13-q28 | No | Unclear | No | ||
| 11q | Loss | 11q14-q23 | No | Unclear | No |
editv4:Genomic Gain/Loss/LOHThe content below was from the old template. Please incorporate above.
Frequent secondary chromosomal imbalances are seen in ALK+ ALCL (58% of cases), as based on comparative genomic hybridization analysis[37].
| Chromosome Number | Gain/Loss/Amp/LOH | Frequency | Comment |
|---|---|---|---|
| 2q | Gain | 12% | |
| 4q | Loss | 28% | |
| 11q22 (ATM) | Loss, LOH | 28% | |
| 13q | Loss | 28% | Also see in ALK- cases |
| 7p | Gain | 12% | Also seen in ALK- cases |
| 17p13 (TP53) | Gain | 28% | |
| 17p13 (TP53) | Loss[38] | 9% | More common in ALK- cases (42%) |
| 17q24-qter | Gain | 28% |
End of V4 Section
Characteristic Chromosomal or Other Global Mutational Patterns
Put your text here and fill in the table (Instructions: Included in this category are alterations such as hyperdiploid; gain of odd number chromosomes including typically chromosome 1, 3, 5, 7, 11, and 17; co-deletion of 1p and 19q; complex karyotypes without characteristic genetic findings; chromothripsis; microsatellite instability; homologous recombination deficiency; mutational signature pattern; etc. Details on clinical significance such as prognosis and other important information can be provided in the notes section. Please include references throughout the table. Do not delete the table.)
| Chromosomal Pattern | Molecular Pathogenesis | Prevalence -
Common >20%, Recurrent 5-20% or Rare <5% (Disease) |
Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | Established Clinical Significance Per Guidelines - Yes or No (Source) | Clinical Relevance Details/Other Notes |
|---|---|---|---|---|---|
| EXAMPLE:
Co-deletion of 1p and 18q |
EXAMPLE: See chromosomal rearrangements table as this pattern is due to an unbalanced derivative translocation associated with oligodendroglioma (add reference). | EXAMPLE: Common (Oligodendroglioma) | EXAMPLE: D, P | ||
| EXAMPLE:
Microsatellite instability - hypermutated |
EXAMPLE: Common (Endometrial carcinoma) | EXAMPLE: P, T | |||
editv4:Characteristic Chromosomal Aberrations / PatternsThe content below was from the old template. Please incorporate above.
See other sections.
End of V4 Section
Gene Mutations (SNV/INDEL)
| Gene | Genetic Alteration | Tumor Suppressor Gene, Oncogene, Other | Prevalence -
Common >20%, Recurrent 5-20% or Rare <5% (Disease) |
Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | Established Clinical Significance Per Guidelines - Yes or No (Source) | Clinical Relevance Details/Other Notes |
|---|---|---|---|---|---|---|
| EXAMPLE:EGFR
|
EXAMPLE: Exon 18-21 activating mutations | EXAMPLE: Oncogene | EXAMPLE: Common (lung cancer) | EXAMPLE: T | EXAMPLE: Yes (NCCN) | EXAMPLE: Exons 18, 19, and 21 mutations are targetable for therapy. Exon 20 T790M variants cause resistance to first generation TKI therapy and are targetable by second and third generation TKIs (add references). |
| EXAMPLE: TP53; Variable LOF mutations
|
EXAMPLE: Variable LOF mutations | EXAMPLE: Tumor Supressor Gene | EXAMPLE: Common (breast cancer) | EXAMPLE: P | EXAMPLE: >90% are somatic; rare germline alterations associated with Li-Fraumeni syndrome (add reference). Denotes a poor prognosis in breast cancer. | |
| EXAMPLE: BRAF; Activating mutations | EXAMPLE: Activating mutations | EXAMPLE: Oncogene | EXAMPLE: Common (melanoma) | EXAMPLE: T | ||
Note: A more extensive list of mutations can be found in cBioportal, COSMIC, and/or other databases. When applicable, gene-specific pages within the CCGA site directly link to pertinent external content.
| Gene; Genetic Alteration | Presumed Mechanism (Tumor Suppressor Gene [TSG] / Oncogene / Other) | Prevalence (COSMIC / TCGA / Other) | Concomitant Mutations | Mutually Exclusive Mutations | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|---|---|---|---|
| LRP1B[39] | TSG | 19% | No | No | No | No | No | |
| NOTCH1[35] | Activating mutation | 9.3% (p.Thr349Pro)
10.2% (p.Thr311Pro) |
No | No | No | No | Yes | May be a biomarker for risk of relapse[35] |
| TP53[39] | TSG | 11% | No | No | No | Yes | No | |
| ALK[40][41][42][43][44][45][46] | Therapeutic Resistance mutations | No | No | No | Yes | ALK kinase domain secondary mutations, including L1196 M, G1269A, L1152R, C1156Y, I1171T, F1174 L, G1202R, and S1206Y, have been identified as the key mechanism of resistance
|
Note: A more extensive list of mutations can be found in cBioportal (https://www.cbioportal.org/), COSMIC (https://cancer.sanger.ac.uk/cosmic), ICGC (https://dcc.icgc.org/) and/or other databases. When applicable, gene-specific pages within the CCGA site directly link to pertinent external content.
editv4:Gene Mutations (SNV/INDEL)The content below was from the old template. Please incorporate above.
- Limited literature on somatic mutations in ALK+ ALCL
| Gene | Function or Presumed Mechanism | Frequency |
|---|---|---|
| LRP1B[39] | Tumor suppressor | 19% |
| NOTCH1[35] | Activating | 9.3% (p.Thr349Pro)
10.2% (p.Thr311Pro) |
| TP53[39] | Tumor suppressor | 11% |
- Epigenetic modifier genes: KMT2D, TET2, EP300, KMT2C[39]
- Other mutations: EPHA5
Negative genes mutations:
- JAK1, STAT3: Mutations described in ALK(-) ALCL[47], and breast implant-associated anaplastic large cell lymphoma (BIA-ALCL)[48]
- RHOA, DNMT3A, CD28: Mutations described in peripheral T cell-lymphoma (PTCL), NOS, and in angioimmunoblastic T-cell lymphoma (AITL)[49]
- IDH2 mutations are relatively specific for AITL[50][51]
A variety of mechanisms for the acquired resistance to ALK inhibitors, such as crizotinib, have been described:
- ALK kinase domain secondary mutations, including L1196 M, G1269A, L1152R, C1156Y, I1171T, F1174 L, G1202R, and S1206Y, have been identified as the key mechanism of resistance[46][40][41][42][43][44][45]
- The G1269A mutation, in which the glycine at 1269 is substituted with an alanine, causes steric hindrance, resulting in decreased affinity for crizotinib.[52][53]
- Gain in ALK copy number and loss of ALK gene rearrangement have also been implicated in the development of acquired resistance to crizotinib.[41][42][43]
End of V4 Section
Epigenomic Alterations
- NPM-ALK via STAT3-activated DNA methyltransferases[54] uses epigenetic silencing mechanisms to:
- Downregulate tumor suppressor genes to maintain its own expression (i.e. to inhibit downregulation of NPM-ALK). Silenced tumor suppressors include:
- Silence T-cell receptor complex and signaling pathway (CD3e, ZAP70, LAT, SLP76)[59]
- Histone H3 lysine 27 (H3K27) trimethylation silences promoters of important T-cell transcription factor genes (GATA3, TCF1 and LEF1)[60]
- Reader is directed to this review for more comprehensive review of epigenetics in peripheral T-cell lymphomas[61]
Genes and Main Pathways Involved
Put your text here and fill in the table (Instructions: Can include references in the table. Do not delete table.)
| Gene; Genetic Alteration | Pathway | Pathophysiologic Outcome |
|---|---|---|
| ALK; fusion protein derivatives | Ras-ERK[62] | Increased cell growth and proliferation |
| ALK; fusion protein derivatives | JAK/STAT3[62] | Cell survival and phenotypic changes |
| ALK; fusion protein derivatives | PI3K/AKT/mTOR[62] | Cell survival and phenotypic changes |
- ALK-NPM-STAT3 induces:
- See Epigenomics section above
- TGF beta, IL-10, PD-L1/CD274 to create immunosuppressive microenvironment and evasion of immune system[63][64][65]
- ICOS expression (CD28 costimulatory receptor superfamily)
- HIF1α expression induces expression of VEGF (tumor angiogenesis); allows lymphoma cells to adapt to hypoxic conditions[66]
- Expression of embryonic genes (SOX2, SALL4) promoting stem cell-like program
- Deregulation of microRNAs (miR-155, miR-101, miR-17-92 cluster, miR-26a, miR-16)[67][68][69][70][71]
editv4:Genes and Main Pathways InvolvedThe content below was from the old template. Please incorporate above.
- Activation of the ALK catalytic domain leads to the oncogenic properties of the ALK protein, leading to activation of multiple signaling cascades including[62]:
- RAS-ERK
- JAK/STAT
- STAT3 is a pivotal transcription factor in most ALCL subtypes:
- NPM1/ALK and variants lead to expression of ALK fusion proteins with constitutive ALK tyrosine kinase activity, which converges in the activation of the downstream oncogenic transcription factor STAT3[47][49].
- In the absence of ALK fusions there are activation JAK1 and/or STAT3 mutations in ALK(-) ALCL [47], and some BIA-ALCL. [72].
- STAT3 is a pivotal transcription factor in most ALCL subtypes:
- PI3K/AKT/mTOR
- ALK-NPM-STAT3 induces:
- See Epigenomics section above
- TGF beta, IL-10, PD-L1/CD274 to create immunosuppressive microenvironment and evasion of immune system[63][64][65]
- ICOS expression (CD28 costimulatory receptor superfamily)
- HIF1α expression induces expression of VEGF (tumor angiogenesis); allows lymphoma cells to adapt to hypoxic conditions[66]
- Expression of embryonic genes (SOX2, SALL4) promoting stem cell-like program
- Deregulation of microRNAs (miR-155, miR-101, miR-17-92 cluster, miR-26a, miR-16)[67][68][69][70][71]
End of V4 Section
Genetic Diagnostic Testing Methods
- Diagnosis is based on histologic evaluation and immunohistochemical positivity for CD30 and ALK on the T-lymphoma cells.
- FISH using an ALK breakapart probe or karyotype analysis can detect ALK translocations, but is not required for diagnosis as it can be established by morphology and immunohistochemistry.
Familial Forms
- None
Additional Information
This disease is defined/characterized as detailed below:
Anaplastic Large Cell Lymphoma, ALK-Positive (ALK+ ALCL) is a T-cell lymphoma characterized by usually large lymphoma cells with abundant cytoplasm and pleomorphic nuclei, often horse-shoe shaped (see Morphologic Features below), with a chromosomal rearrangement involving the ALK gene resulting in expression of ALK protein and CD30
The epidemiology/prevalence of this disease is detailed below:
- ALCL (ALK+, ALK-, and primary cutaneous) account for <5% of all cases of non-Hodgkin lymphoma (NHL)[4]
- ALK+ ALCL[4]
- ~3% of adult NHL
- 10-20% of childhood lymphomas
- Most frequent in the first three decades of life
- Male:female = 1.5:1
The clinical features of this disease are detailed below:
Signs and symptoms - Most patients (70%) present with advanced (stage III-IV) disease and B-symptoms.[73]
Laboratory findings - Noncontributory
The sites of involvement of this disease are detailed below:
- Lymph nodes and extranodal sites (most commonly skin, bone, soft tissue, lungs and liver)[4]
- Bone marrow involvement detected in 30% when using immunohistochemistry (CD30 and EMA). Can miss marrow involvement by H&E evaluation alone, which detects involvement with ~10% incidence.[74]
The morphologic features of this disease are detailed below:
- Lymphoma cells characterized by eccentric, horseshoe-shaped or kidney-shaped nuclei, often with eosinophilic cytoplasm accentuated near the nucleus
- Usually large in size, but may also be smaller
- Present in varying proportions
- Seen in all morphological variants/patterns of ALK+ ALCL
Morphological variants/patterns
- Common (60%): predominant population of large hallmark cells
- Lymphohistiocytic (10%): lymphoma cells are admixed with numerous reactive histiocytes that may obscure the lymphoma cells; lymphoma cells often cluster around vessels and are often smaller than in the common pattern
- Small cell (5-10%): predominant population of smaller lymphoma cells; hallmark cells are often concentrated around vessels; may also see "fried egg cells" (pale cytoplasm with central nucleus) or signet ring-like cells; can misdiagnose of peripheral T-cell lymphoma, NOS
- Hodgkin-like (3%): mimics nodular sclerosis classic Hodgkin lymphoma
- Composite (15%): more than one pattern in a single lymph node
When lymph node is only partially involved, lymphoma characteristically grows in the sinuses, which may mimic a metastatic tumor.
The immunophenotype of this disease is detailed below:
- CD30 expression on ALCL (ALK+ or ALK-) allows for targeted therapy[7]. First-line therapy: Brentuximab (anti-CD30) vedotin + CHP (cyclophosphamide, doxorubicin, and prednisone)
CD30+: Positive (universal) - cell membrane and Golgi; large lymphoma cells show strongest staining; smaller cells may show weak, partial to negative staining
ALK: Positive (universal) - cellular location of ALK staining varies depending on ALK translocation partner. In the most common t(2;5), most cases show both cytoplasmic and nuclear
EMA: positive (subset)
CD3: Positive (subset)
CD4: Positive (70%)
CD5: Negative in majority of cases
CD8: Positive in majority of cases
CD2: Positive in majority of cases
TIA1: Positive
Granzyme B: Positive
Perforin: Positive
CD45: Variably positive
CD25: Positive (universal)
BCL2: Negative (universal)
Links
- See References.
References
(use the "Cite" icon at the top of the page) (Instructions: Add each reference into the text above by clicking where you want to insert the reference, selecting the “Cite” icon at the top of the wiki page, and using the “Automatic” tab option to search by PMID to select the reference to insert. If a PMID is not available, such as for a book, please use the “Cite” icon, select “Manual” and then “Basic Form”, and include the entire reference. To insert the same reference again later in the page, select the “Cite” icon and “Re-use” to find the reference; DO NOT insert the same reference twice using the “Automatic” tab as it will be treated as two separate references. The reference list in this section will be automatically generated and sorted.)
- ↑ 1.0 1.1 Falini, B.; et al. (1998-09). "ALK expression defines a distinct group of T/null lymphomas ("ALK lymphomas") with a wide morphological spectrum". The American Journal of Pathology. 153 (3): 875–886. doi:10.1016/S0002-9440(10)65629-5. ISSN 0002-9440. PMC 1853018. PMID 9736036. Check date values in:
|date=(help) - ↑ 2.0 2.1 Pittaluga, S.; et al. (1997-08). "The monoclonal antibody ALK1 identifies a distinct morphological subtype of anaplastic large cell lymphoma associated with 2p23/ALK rearrangements". The American Journal of Pathology. 151 (2): 343–351. ISSN 0002-9440. PMC 1858018. PMID 9250148. Check date values in:
|date=(help) - ↑ 3.0 3.1 Morris, S. W.; et al. (1994-03-04). "Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin's lymphoma". Science (New York, N.Y.). 263 (5151): 1281–1284. doi:10.1126/science.8122112. ISSN 0036-8075. PMID 8122112.
- ↑ 4.0 4.1 4.2 4.3 Arber DA, et al., (2017). Anaplastic large cell lymphoma, ALK-positive, in World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues, Revised 4th edition. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Arber DA, Hasserjian RP, Le Beau MM, Orazi A, and Siebert R, Editors. IARC Press: Lyon, France, p413-418.
- ↑ 5.0 5.1 C, Damm-Welk; et al. (2014). "Early assessment of minimal residual disease identifies patients at very high relapse risk in NPM-ALK-positive anaplastic large-cell lymphoma". PMID 24297868.
- ↑ 6.0 6.1 Werner, Michael T.; et al. (02 16, 2017). "Nucleophosmin-anaplastic lymphoma kinase: the ultimate oncogene and therapeutic target". Blood. 129 (7): 823–831. doi:10.1182/blood-2016-05-717793. ISSN 1528-0020. PMID 27879258. Check date values in:
|date=(help) - ↑ 7.0 7.1 7.2 7.3 National Comprehensive Cancer Network (January 2021). "NCCN Clinical Practice Guidelines in Oncology: T-cell lymphomas" (PDF).CS1 maint: display-authors (link)
- ↑ 8.0 8.1 Food and Drug Administration (January 2021). "FDA approves crizotinib for children and young adults with relapsed or refractory, systemic anaplastic large cell lymphoma".CS1 maint: display-authors (link)
- ↑ 9.0 9.1 9.2 Zdzalik, Daria; et al. (2014-04). "Activating mutations in ALK kinase domain confer resistance to structurally unrelated ALK inhibitors in NPM-ALK-positive anaplastic large-cell lymphoma". Journal of Cancer Research and Clinical Oncology. 140 (4): 589–598. doi:10.1007/s00432-014-1589-3. ISSN 1432-1335. PMC 3949014. PMID 24509625. Check date values in:
|date=(help) - ↑ 10.0 10.1 10.2 Lamant, L.; et al. (1999-05-01). "A new fusion gene TPM3-ALK in anaplastic large cell lymphoma created by a (1;2)(q25;p23) translocation". Blood. 93 (9): 3088–3095. ISSN 0006-4971. PMID 10216106.
- ↑ 11.0 11.1 11.2 Trinei, M.; et al. (2000-02-15). "A new variant anaplastic lymphoma kinase (ALK)-fusion protein (ATIC-ALK) in a case of ALK-positive anaplastic large cell lymphoma". Cancer Research. 60 (4): 793–798. ISSN 0008-5472. PMID 10706082.
- ↑ 12.0 12.1 Hernández, L.; et al. (1999-11-01). "TRK-fused gene (TFG) is a new partner of ALK in anaplastic large cell lymphoma producing two structurally different TFG-ALK translocations". Blood. 94 (9): 3265–3268. ISSN 0006-4971. PMID 10556217.
- ↑ 13.0 13.1 Touriol, C.; et al. (2000-05-15). "Further demonstration of the diversity of chromosomal changes involving 2p23 in ALK-positive lymphoma: 2 cases expressing ALK kinase fused to CLTCL (clathrin chain polypeptide-like)". Blood. 95 (10): 3204–3207. ISSN 0006-4971. PMID 10807789.
- ↑ 14.0 14.1 Tort, F.; et al. (2001-03). "Molecular characterization of a new ALK translocation involving moesin (MSN-ALK) in anaplastic large cell lymphoma". Laboratory Investigation; a Journal of Technical Methods and Pathology. 81 (3): 419–426. doi:10.1038/labinvest.3780249. ISSN 0023-6837. PMID 11310834. Check date values in:
|date=(help) - ↑ 15.0 15.1 15.2 15.3 Cools, Jan; et al. (2002-08). "Identification of novel fusion partners of ALK, the anaplastic lymphoma kinase, in anaplastic large-cell lymphoma and inflammatory myofibroblastic tumor". Genes, Chromosomes & Cancer. 34 (4): 354–362. doi:10.1002/gcc.10033. ISSN 1045-2257. PMID 12112524. Check date values in:
|date=(help) - ↑ 16.0 16.1 Lamant, Laurence; et al. (2003-08). "Non-muscle myosin heavy chain (MYH9): a new partner fused to ALK in anaplastic large cell lymphoma". Genes, Chromosomes & Cancer. 37 (4): 427–432. doi:10.1002/gcc.10232. ISSN 1045-2257. PMID 12800156. Check date values in:
|date=(help) - ↑ 17.0 17.1 Feldman, Andrew L.; et al. (2013-11). "Novel TRAF1-ALK fusion identified by deep RNA sequencing of anaplastic large cell lymphoma". Genes, Chromosomes & Cancer. 52 (11): 1097–1102. doi:10.1002/gcc.22104. ISSN 1098-2264. PMID 23999969. Check date values in:
|date=(help) - ↑ Holla, Vijaykumar R.; et al. (2017-1). "ALK: a tyrosine kinase target for cancer therapy". Cold Spring Harbor Molecular Case Studies. 3 (1): a001115. doi:10.1101/mcs.a001115. ISSN 2373-2873. PMC 5171696. PMID 28050598. Check date values in:
|date=(help) - ↑ Amatu, Alessio; et al. (2015-12-22). "Novel CAD-ALK gene rearrangement is drugable by entrectinib in colorectal cancer". British Journal of Cancer. 113 (12): 1730–1734. doi:10.1038/bjc.2015.401. ISSN 0007-0920. PMC 4701996. PMID 26633560.
- ↑ Camidge, D. Ross; et al. (2011-04). "Anaplastic lymphoma kinase gene rearrangements in non-small cell lung cancer are associated with prolonged progression-free survival on pemetrexed". Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer. 6 (4): 774–780. doi:10.1097/JTO.0b013e31820cf053. ISSN 1556-1380. PMC 3626562. PMID 21336183. Check date values in:
|date=(help) - ↑ Choi, Young Lim; et al. (2008-07-01). "Identification of novel isoforms of the EML4-ALK transforming gene in non-small cell lung cancer". Cancer Research. 68 (13): 4971–4976. doi:10.1158/0008-5472.CAN-07-6158. ISSN 1538-7445. PMID 18593892.
- ↑ Kelly, Lindsey M.; et al. (2014-03-18). "Identification of the transforming STRN-ALK fusion as a potential therapeutic target in the aggressive forms of thyroid cancer". Proceedings of the National Academy of Sciences of the United States of America. 111 (11): 4233–4238. doi:10.1073/pnas.1321937111. ISSN 0027-8424. PMC 3964116. PMID 24613930.
- ↑ Ambrosini, Margherita; et al. (2022-04). "ALK Inhibitors in Patients With ALK Fusion-Positive GI Cancers: An International Data Set and a Molecular Case Series". JCO precision oncology. 6: e2200015. doi:10.1200/PO.22.00015. ISSN 2473-4284. PMID 35476549 Check
|pmid=value (help). Check date values in:|date=(help) - ↑ Bridge, Julia A.; et al. (2001-8). "Fusion of the ALK Gene to the Clathrin Heavy Chain Gene, CLTC, in Inflammatory Myofibroblastic Tumor". The American Journal of Pathology. 159 (2): 411–415. ISSN 0002-9440. PMC 1850566. PMID 11485898. Check date values in:
|date=(help) - ↑ Lawrence, B.; et al. (2000-08). "TPM3-ALK and TPM4-ALK oncogenes in inflammatory myofibroblastic tumors". The American Journal of Pathology. 157 (2): 377–384. doi:10.1016/S0002-9440(10)64550-6. ISSN 0002-9440. PMC 1850130. PMID 10934142. Check date values in:
|date=(help) - ↑ Ma, Zhigui; et al. (2003-05). "Fusion of ALK to the Ran-binding protein 2 (RANBP2) gene in inflammatory myofibroblastic tumor". Genes, Chromosomes & Cancer. 37 (1): 98–105. doi:10.1002/gcc.10177. ISSN 1045-2257. PMID 12661011. Check date values in:
|date=(help) - ↑ Pan, Zenggang; et al. (2017-01). "ALK-positive Large B-cell Lymphoma: A Clinicopathologic Study of 26 Cases With Review of Additional 108 Cases in the Literature". The American Journal of Surgical Pathology. 41 (1): 25–38. doi:10.1097/PAS.0000000000000753. ISSN 1532-0979. PMID 27740969. Check date values in:
|date=(help) - ↑ Laurent, Camille; et al. (2009-09-01). "Anaplastic lymphoma kinase-positive diffuse large B-cell lymphoma: a rare clinicopathologic entity with poor prognosis". Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 27 (25): 4211–4216. doi:10.1200/JCO.2008.21.5020. ISSN 1527-7755. PMID 19636007.
- ↑ Sakamoto, Kana; et al. (2016-04). "ALK-positive large B-cell lymphoma: identification of EML4-ALK and a review of the literature focusing on the ALK immunohistochemical staining pattern". International Journal of Hematology. 103 (4): 399–408. doi:10.1007/s12185-016-1934-1. ISSN 1865-3774. PMID 26781614. Check date values in:
|date=(help) - ↑ Takeyasu, Yuki; et al. (2021). "Impact of ALK Inhibitors in Patients With ALK-Rearranged Nonlung Solid Tumors". JCO precision oncology. 5: PO.20.00383. doi:10.1200/PO.20.00383. ISSN 2473-4284. PMC 8140781 Check
|pmc=value (help). PMID 34036223 Check|pmid=value (help). - ↑ Chang, Kenneth Tou En; et al. (2019-05). "ALK-positive histiocytosis: an expanded clinicopathologic spectrum and frequent presence of KIF5B-ALK fusion". Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc. 32 (5): 598–608. doi:10.1038/s41379-018-0168-6. ISSN 1530-0285. PMID 30573850. Check date values in:
|date=(help) - ↑ Chan, John K. C.; et al. (2008-10-01). "ALK+ histiocytosis: a novel type of systemic histiocytic proliferative disorder of early infancy". Blood. 112 (7): 2965–2968. doi:10.1182/blood-2008-03-147017. ISSN 1528-0020. PMID 18660380.
- ↑ D, Sibon; et al. (2012). "Long-term outcome of adults with systemic anaplastic large-cell lymphoma treated within the Groupe d'Etude des Lymphomes de l'Adulte trials". PMID 23045585.
- ↑ L, Lamant; et al. (2011). "Prognostic impact of morphologic and phenotypic features of childhood ALK-positive anaplastic large-cell lymphoma: results of the ALCL99 study". PMID 22084369.
- ↑ 35.0 35.1 35.2 35.3 35.4 Larose, Hugo; et al. (04 23, 2020). "Whole Exome Sequencing reveals NOTCH1 mutations in anaplastic large cell lymphoma and points to Notch both as a key pathway and a potential therapeutic target". Haematologica. doi:10.3324/haematol.2019.238766. ISSN 1592-8721. PMID 32327503 Check
|pmid=value (help). Check date values in:|date=(help) - ↑ Rozati, Sima; et al. (2016-04-15). "Romidepsin and Azacitidine Synergize in their Epigenetic Modulatory Effects to Induce Apoptosis in CTCL". Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 22 (8): 2020–2031. doi:10.1158/1078-0432.CCR-15-1435. ISSN 1557-3265. PMID 26660520.
- ↑ I, Salaverria; et al. (2008). "Genomic profiling reveals different genetic aberrations in systemic ALK-positive and ALK-negative anaplastic large cell lymphomas". PMID 18275429.
- ↑ Boi, Michela; et al. (2013-10-10). "PRDM1/BLIMP1 is commonly inactivated in anaplastic large T-cell lymphoma". Blood. 122 (15): 2683–2693. doi:10.1182/blood-2013-04-497933. ISSN 0006-4971.
- ↑ 39.0 39.1 39.2 39.3 39.4 Lobello, Cosimo; et al. (2020-11-27). "STAT3 and TP53 mutations associate with poor prognosis in anaplastic large cell lymphoma". Leukemia: 1–6. doi:10.1038/s41375-020-01093-1. ISSN 1476-5551.
- ↑ 40.0 40.1 Gainor, Justin F.; et al. (2013-08-01). "ALK rearrangements are mutually exclusive with mutations in EGFR or KRAS: an analysis of 1,683 patients with non-small cell lung cancer". Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 19 (15): 4273–4281. doi:10.1158/1078-0432.CCR-13-0318. ISSN 1557-3265. PMC 3874127. PMID 23729361.
- ↑ 41.0 41.1 41.2 Doebele, Robert C.; et al. (2012-03-01). "Mechanisms of resistance to crizotinib in patients with ALK gene rearranged non-small cell lung cancer". Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 18 (5): 1472–1482. doi:10.1158/1078-0432.CCR-11-2906. ISSN 1557-3265. PMC 3311875. PMID 22235099.
- ↑ 42.0 42.1 42.2 Isozaki, Hideko; et al. (2015-04-30). "Mechanisms of Acquired Resistance to ALK Inhibitors and the Rationale for Treating ALK-positive Lung Cancer". Cancers. 7 (2): 763–783. doi:10.3390/cancers7020763. ISSN 2072-6694. PMC 4491683. PMID 25941796.
- ↑ 43.0 43.1 43.2 Sasaki, Takaaki; et al. (2011-09-15). "A novel ALK secondary mutation and EGFR signaling cause resistance to ALK kinase inhibitors". Cancer Research. 71 (18): 6051–6060. doi:10.1158/0008-5472.CAN-11-1340. ISSN 1538-7445. PMC 3278914. PMID 21791641.
- ↑ 44.0 44.1 Toyokawa, Gouji; et al. (2014-12). "Secondary mutations at I1171 in the ALK gene confer resistance to both Crizotinib and Alectinib". Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer. 9 (12): e86–87. doi:10.1097/JTO.0000000000000358. ISSN 1556-1380. PMID 25393798. Check date values in:
|date=(help) - ↑ 45.0 45.1 Li, Yanrong; et al. (2020-06). "Activation of IGF-1R pathway and NPM-ALK G1269A mutation confer resistance to crizotinib treatment in NPM-ALK positive lymphoma". Investigational New Drugs. 38 (3): 599–609. doi:10.1007/s10637-019-00802-7. ISSN 1573-0646. PMID 31177400. Check date values in:
|date=(help) - ↑ 46.0 46.1 Guérin, Annie; et al. (2015-06). "ALK rearrangement testing and treatment patterns for patients with ALK-positive non-small cell lung cancer". Cancer Epidemiology. 39 (3): 307–312. doi:10.1016/j.canep.2015.04.005. ISSN 1877-783X. PMID 25914136. Check date values in:
|date=(help) - ↑ 47.0 47.1 47.2 Crescenzo, Ramona; et al. (2015-04-13). "Convergent mutations and kinase fusions lead to oncogenic STAT3 activation in anaplastic large cell lymphoma". Cancer Cell. 27 (4): 516–532. doi:10.1016/j.ccell.2015.03.006. ISSN 1878-3686. PMC 5898430. PMID 25873174.
- ↑ Blombery, Piers; et al. (2016-9). "Whole exome sequencing reveals activating JAK1 and STAT3 mutations in breast implant-associated anaplastic large cell lymphoma anaplastic large cell lymphoma". Haematologica. 101 (9): e387–e390. doi:10.3324/haematol.2016.146118. ISSN 0390-6078. PMC 5060038. PMID 27198716. Check date values in:
|date=(help) - ↑ 49.0 49.1 Sandell, Rosalind F.; et al. (2017-04). "Genetic Landscape and Classification of Peripheral T Cell Lymphomas". Current Oncology Reports. 19 (4): 28. doi:10.1007/s11912-017-0582-9. ISSN 1534-6269. PMC 5517131. PMID 28303495. Check date values in:
|date=(help) - ↑ Wang, Chao; et al. (2015-10-08). "IDH2R172 mutations define a unique subgroup of patients with angioimmunoblastic T-cell lymphoma". Blood. 126 (15): 1741–1752. doi:10.1182/blood-2015-05-644591. ISSN 1528-0020. PMC 4600014. PMID 26268241.
- ↑ Cairns, Rob A.; et al. (2012-02-23). "IDH2 mutations are frequent in angioimmunoblastic T-cell lymphoma". Blood. 119 (8): 1901–1903. doi:10.1182/blood-2011-11-391748. ISSN 1528-0020. PMC 3293643. PMID 22215888.
- ↑ Friboulet, Luc; et al. (2014-06). "The ALK inhibitor ceritinib overcomes crizotinib resistance in non-small cell lung cancer". Cancer Discovery. 4 (6): 662–673. doi:10.1158/2159-8290.CD-13-0846. ISSN 2159-8290. PMC 4068971. PMID 24675041. Check date values in:
|date=(help) - ↑ Alshareef, Abdulraheem; et al. (2016-09-19). "The use of cellular thermal shift assay (CETSA) to study Crizotinib resistance in ALK-expressing human cancers". Scientific Reports. 6: 33710. doi:10.1038/srep33710. ISSN 2045-2322. PMC 5027386. PMID 27641368.
- ↑ Zhang, Qian; et al. (2006-08-01). "STAT3 induces transcription of the DNA methyltransferase 1 gene (DNMT1) in malignant T lymphocytes". Blood. 108 (3): 1058–1064. doi:10.1182/blood-2005-08-007377. ISSN 0006-4971. PMC 1895864. PMID 16861352.
- ↑ Zhang, Qian; et al. (2007-11). "STAT5A is epigenetically silenced by the tyrosine kinase NPM1-ALK and acts as a tumor suppressor by reciprocally inhibiting NPM1-ALK expression". Nature Medicine. 13 (11): 1341–1348. doi:10.1038/nm1659. ISSN 1078-8956. PMID 17922009. Check date values in:
|date=(help) - ↑ Zhang, Qian; et al. (2005-05-10). "STAT3- and DNA methyltransferase 1-mediated epigenetic silencing of SHP-1 tyrosine phosphatase tumor suppressor gene in malignant T lymphocytes". Proceedings of the National Academy of Sciences of the United States of America. 102 (19): 6948–6953. doi:10.1073/pnas.0501959102. ISSN 0027-8424. PMC 1100783. PMID 15870198.
- ↑ 57.0 57.1 Zhang, Qian; et al. (2011-07-19). "IL-2R common gamma-chain is epigenetically silenced by nucleophosphin-anaplastic lymphoma kinase (NPM-ALK) and acts as a tumor suppressor by targeting NPM-ALK". Proceedings of the National Academy of Sciences of the United States of America. 108 (29): 11977–11982. doi:10.1073/pnas.1100319108. ISSN 1091-6490. PMC 3141982. PMID 21715655.
- ↑ Hoareau-Aveilla, Coralie; et al. (2015-09). "Reversal of microRNA-150 silencing disadvantages crizotinib-resistant NPM-ALK(+) cell growth". The Journal of Clinical Investigation. 125 (9): 3505–3518. doi:10.1172/JCI78488. ISSN 1558-8238. PMC 4588301. PMID 26258416. Check date values in:
|date=(help) - ↑ Ambrogio, Chiara; et al. (2009-11-15). "NPM-ALK oncogenic tyrosine kinase controls T-cell identity by transcriptional regulation and epigenetic silencing in lymphoma cells". Cancer Research. 69 (22): 8611–8619. doi:10.1158/0008-5472.CAN-09-2655. ISSN 1538-7445. PMC 2784121. PMID 19887607.
- ↑ Joosten, Maria; et al. (2013-02). "Histone acetylation and DNA demethylation of T cells result in an anaplastic large cell lymphoma-like phenotype". Haematologica. 98 (2): 247–254. doi:10.3324/haematol.2011.054619. ISSN 1592-8721. PMC 3561432. PMID 22899583. Check date values in:
|date=(help) - ↑ Zhang, Ping; et al. (2020-11-07). "Epigenetic alterations and advancement of treatment in peripheral T-cell lymphoma". Clinical Epigenetics. 12 (1): 169. doi:10.1186/s13148-020-00962-x. ISSN 1868-7083. PMC 7648940 Check
|pmc=value (help). PMID 33160401 Check|pmid=value (help). - ↑ 62.0 62.1 62.2 62.3 M, Boi; et al. (2015). "Advances in understanding the pathogenesis of systemic anaplastic large cell lymphomas". PMID 25559471.
- ↑ 63.0 63.1 Marzec, Michal; et al. (2008-12-30). "Oncogenic kinase NPM/ALK induces through STAT3 expression of immunosuppressive protein CD274 (PD-L1, B7-H1)". Proceedings of the National Academy of Sciences of the United States of America. 105 (52): 20852–20857. doi:10.1073/pnas.0810958105. ISSN 1091-6490. PMC 2634900. PMID 19088198.
- ↑ 64.0 64.1 Kasprzycka, Monika; et al. (2008-08-15). "Gamma c-signaling cytokines induce a regulatory T cell phenotype in malignant CD4+ T lymphocytes". Journal of Immunology (Baltimore, Md.: 1950). 181 (4): 2506–2512. doi:10.4049/jimmunol.181.4.2506. ISSN 1550-6606. PMC 2586884. PMID 18684941.
- ↑ 65.0 65.1 Yamamoto, Ryo; et al. (2009-11). "B7-H1 expression is regulated by MEK/ERK signaling pathway in anaplastic large cell lymphoma and Hodgkin lymphoma". Cancer Science. 100 (11): 2093–2100. doi:10.1111/j.1349-7006.2009.01302.x. ISSN 1349-7006. PMID 19703193. Check date values in:
|date=(help) - ↑ 66.0 66.1 Martinengo, Cinzia; et al. (2014-11-01). "ALK-dependent control of hypoxia-inducible factors mediates tumor growth and metastasis". Cancer Research. 74 (21): 6094–6106. doi:10.1158/0008-5472.CAN-14-0268. ISSN 1538-7445. PMID 25193384.
- ↑ 67.0 67.1 Rodriguez, Antony; et al. (2007-04-27). "Requirement of bic/microRNA-155 for normal immune function". Science (New York, N.Y.). 316 (5824): 608–611. doi:10.1126/science.1139253. ISSN 1095-9203. PMC 2610435. PMID 17463290.
- ↑ 68.0 68.1 Merkel, Olaf; et al. (2010-09-14). "Identification of differential and functionally active miRNAs in both anaplastic lymphoma kinase (ALK)+ and ALK- anaplastic large-cell lymphoma". Proceedings of the National Academy of Sciences of the United States of America. 107 (37): 16228–16233. doi:10.1073/pnas.1009719107. ISSN 1091-6490. PMC 2941277. PMID 20805506.
- ↑ 69.0 69.1 Spaccarotella, Elisa; et al. (2014-01). "STAT3-mediated activation of microRNA cluster 17~92 promotes proliferation and survival of ALK-positive anaplastic large cell lymphoma". Haematologica. 99 (1): 116–124. doi:10.3324/haematol.2013.088286. ISSN 1592-8721. PMC 4007939. PMID 23975180. Check date values in:
|date=(help) - ↑ 70.0 70.1 Zhu, Haifeng; et al. (2013-05). "NPM-ALK up-regulates iNOS expression through a STAT3/microRNA-26a-dependent mechanism". The Journal of Pathology. 230 (1): 82–94. doi:10.1002/path.4171. ISSN 1096-9896. PMC 3940725. PMID 23338972. Check date values in:
|date=(help) - ↑ 71.0 71.1 Dejean, E.; et al. (2011-12). "Hypoxia-microRNA-16 downregulation induces VEGF expression in anaplastic lymphoma kinase (ALK)-positive anaplastic large-cell lymphomas". Leukemia. 25 (12): 1882–1890. doi:10.1038/leu.2011.168. ISSN 1476-5551. PMID 21778999. Check date values in:
|date=(help) - ↑ Di Napoli, Arianna; et al. (2018-03). "Targeted next generation sequencing of breast implant-associated anaplastic large cell lymphoma reveals mutations in JAK/STAT signalling pathway genes, TP53 and DNMT3A". British Journal of Haematology. 180 (5): 741–744. doi:10.1111/bjh.14431. ISSN 1365-2141. PMID 27859003. Check date values in:
|date=(help) - ↑ Savage, Kerry J.; et al. (2008-06-15). "ALK- anaplastic large-cell lymphoma is clinically and immunophenotypically different from both ALK+ ALCL and peripheral T-cell lymphoma, not otherwise specified: report from the International Peripheral T-Cell Lymphoma Project". Blood. 111 (12): 5496–5504. doi:10.1182/blood-2008-01-134270. ISSN 1528-0020. PMID 18385450.
- ↑ M, Fraga; et al. (1995). "Bone marrow involvement in anaplastic large cell lymphoma. Immunohistochemical detection of minimal disease and its prognostic significance". PMID 7817951.
- ↑ Stein, H.; et al. (2000-12-01). "CD30(+) anaplastic large cell lymphoma: a review of its histopathologic, genetic, and clinical features". Blood. 96 (12): 3681–3695. ISSN 0006-4971. PMID 11090048.
- ↑ Benharroch, D.; et al. (1998-03-15). "ALK-positive lymphoma: a single disease with a broad spectrum of morphology". Blood. 91 (6): 2076–2084. ISSN 0006-4971. PMID 9490693.
Notes
*Primary authors will typically be those that initially create and complete the content of a page. If a subsequent user modifies the content and feels the effort put forth is of high enough significance to warrant listing in the authorship section, please contact the Associate Editor or other CCGA representative. When pages have a major update, the new author will be acknowledged at the beginning of the page, and those who contributed previously will be acknowledged below as a prior author.
Prior Author(s):
*Citation of this Page: “ALK-positive anaplastic large cell lymphoma”. Compendium of Cancer Genome Aberrations (CCGA), Cancer Genomics Consortium (CGC), updated 09/4/2025, https://ccga.io/index.php/HAEM5:ALK-positive_anaplastic_large_cell_lymphoma.