Acute myeloid leukaemia with BCR::ABL1 fusion
Haematolymphoid Tumours (WHO Classification, 5th ed.)
| This page is under construction |
editContent Update To WHO 5th Edition Classification Is In Process; Content Below is Based on WHO 4th Edition ClassificationThis page was converted to the new template on 2023-12-07. The original page can be found at HAEM4:Acute Myeloid Leukemia (AML) with BCR-ABL1.
(General Instructions – The focus of these pages is the clinically significant genetic alterations in each disease type. This is based on up-to-date knowledge from multiple resources such as PubMed and the WHO classification books. The CCGA is meant to be a supplemental resource to the WHO classification books; the CCGA captures in a continually updated wiki-stye manner the current genetics/genomics knowledge of each disease, which evolves more rapidly than books can be revised and published. If the same disease is described in multiple WHO classification books, the genetics-related information for that disease will be consolidated into a single main page that has this template (other pages would only contain a link to this main page). Use HUGO-approved gene names and symbols (italicized when appropriate), HGVS-based nomenclature for variants, as well as generic names of drugs and testing platforms or assays if applicable. Please complete tables whenever possible and do not delete them (add N/A if not applicable in the table and delete the examples); to add (or move) a row or column in a table, click nearby within the table and select the > symbol that appears. Please do not delete or alter the section headings. The use of bullet points alongside short blocks of text rather than only large paragraphs is encouraged. Additional instructions below in italicized blue text should not be included in the final page content. Please also see Author_Instructions and FAQs as well as contact your Associate Editor or Technical Support.)
Primary Author(s)*
Xinxiu Xu PhD, PharmB, Vanderbilt University Medical Center
WHO Classification of Disease
| Structure | Disease |
|---|---|
| Book | Haematolymphoid Tumours (5th ed.) |
| Category | Myeloid proliferations and neoplasms |
| Family | Acute myeloid leukaemia |
| Type | Acute myeloid leukaemia with defining genetic abnormalities |
| Subtype(s) | Acute myeloid leukaemia with BCR::ABL1 fusion |
Related Terminology
| Acceptable | Acute myeloid leukaemia with t(9;22)(q34;q11.2) |
| Not Recommended | N/A |
Gene Rearrangements
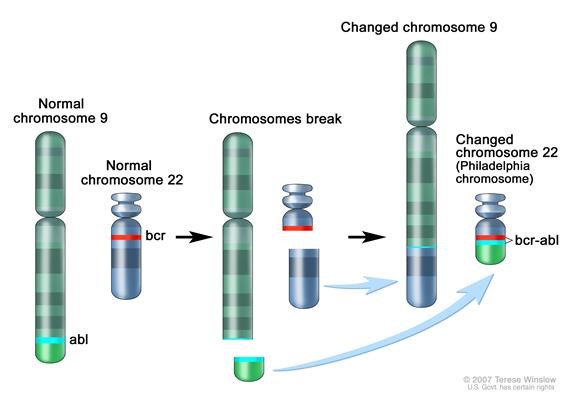
The t(9:22)(q34.1;q11.2) results in the formation of the Ph chromosome and the chimeric BCR-ABL1 fusion gene. In AML, ~70 - 80% cases with BCR::ABL1 harbor p210 transcripts, and 50-60% cases with additional chromosomal abnormalities[1][2][3][4]. The most common BCR-ABL1 transcripts p190 and p210 have been detected in nearly equal distribution[5]. Since p190 is very rare in CML (p210 transcripts in >99% of cases), the presentation with a p190 transcript is in favor of the diagnosis of AML rather than CML[6].
| Driver Gene | Fusion(s) and Common Partner Genes | Molecular Pathogenesis | Typical Chromosomal Alteration(s) | Prevalence -Common >20%, Recurrent 5-20% or Rare <5% (Disease) | Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | Established Clinical Significance Per Guidelines - Yes or No (Source) | Clinical Relevance Details/Other Notes |
|---|---|---|---|---|---|---|---|
| ABL1 | BCR::ABL1 | The pathogenic derivative is the der(22) resulting in fusion of 5’ BCR and 3’ABL1. | t(9;22)(q34;q11.2) | Common (CML); Rare (AML). | Diagnosis: BCR-ABL1 positive AML is an emerging entity. The proliferation of BCR-ABL1 positive blasts present a diagnostic dilemma. While it may be difficult, it is essential to distinguish between BCR-ABL1 positive AML and Chronic Myeloid Leukemia in Myeloid Blast Crisis (CML-MBC), in order to choose the most appropriate therapy (e.g., intensive induction chemotherapy versus tyrosine kinase inhibitor (TKI) followed by an early allogeneic stem cell transplant). After the exclusion of acute leukemia of ambiguous lineage (a separate entity according to WHO) by flow cytometry, it is helpful to note any past history of antecedent hematological disease. Compared to CML-MBC, a higher percentage of blasts (median: 47% vs 13%), a lower percentage of basophils (median: 0% vs 2.5%) and absolute basophil count, a lower frequency of splenomegaly (25% vs 65%), lower cellularity, fewer dwarf megakaryocytes, and normal M:E ratio favor the diagnosis of BCR-ABL1 positive AML[2][1]. The detection of p190 transcript and the occurrence of any BCR-ABL1 transcript in less than 100% of metaphases supports the diagnosis of AML rather than CML. Persistent CCyR (Complete Cytogenetic Response) after conventional chemotherapy is unusual for CML-MBC and supports the diagnosis of BCR-ABL1 positive AML[5]. Karyotype analysis that identifies the t(9;22)(q34;q11.2) translocation, either alone or in conjunction with additional chromosomal abnormalities, characterizes BCR-ABL1 positive AML[1][2]. In addition, molecular methods including dual-colour dual-fusion FISH, RT-PCR, qPCR, and RNA or DNA sequencing are used to identify all common breakpoint variants when applicable.
|
Yes (WHO, NCCN) | The t(9;22) is diagnostic of CML in the appropriate morphology and clinical context[10][11]. The prevalence of BCR"" ABL1 in CML is common ~90-95%[12]. This fusion is responsive to targeted therapy such as Imatinib (Gleevec)[13].
Three BCR-ABL chimeric proteins result from varying mRNA fusions of the ABL and BCR genes. The most common breakpoint occurs in BCR intron 13 or 14, fusing to ABL1 exon a2 (e13a2, e14a2), yielding a 210 kilodalton protein (p210 BCR-ABL1) found in 95% of CML cases. A rare alternative (<1%) is the e19a2 fusion, producing a 230 kilodalton protein (p230 BCR-ABL1), a marker for neutrophilic-chronic myeloid leukemia. The e1a2 fusion results in the p190 BCR-ABL1 protein, prevalent in B cell ALL, less common in AML, and rare in CML[16].
There is a single case report of an AML patient with BCR::ABL1 achieving molecular remission with dasatinib and chemotherapy[18].
|
Individual Region Genomic Gain/Loss/LOH
AML with BCR-ABL1 carries unique genome imbalances. Nacheva et al., used array comparative genomic hybridization (CGH) to perform a comparative study between several BCR-ABL1 positive entities. BCR-ABL1 positive AML displays characteristic of lymphoid disease (found in BCR-ABL1 positive ALL and CML): deletions of IKZF1 and/or CDKN2A/B genes were recurrent findings in BCR-ABL1 positive AML as well as cryptic deletions within the immunoglobulin IGH and T cell receptor gene (TRG alpha) complexes[21]. Importantly, these aberrations were found to be absent in CML-MBC and hence they are potentially a helpful diagnostic tool for difficult cases.
Most cases will have monosomy 7/Del(7q), trisomy 8 or complex karyotypes in addition to the t(9;22)(q34.1;q11.2)[22].
| Chr # | Gain, Loss, Amp, LOH | Minimal Region Cytoband and/or Genomic Coordinates [Genome Build; Size] | Relevant Gene(s) | Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | Established Clinical Significance Per Guidelines - Yes or No (Source) | Clinical Relevance Details/Other Notes |
|---|---|---|---|---|---|---|
| 7 | Loss | chr7 | IKZF1, TR Beta Chain (TRB) genes | D,P | No | Presence of monosomy 7 (or 7q deletion) is sufficient for a diagnosis of AML with MDS-related changes when there is ≥20% blasts and no prior therapy (add reference). Monosomy 7/7q deletion is associated with a poor prognosis in AML[8]. |
| 8 | Gain | chr8 | Unknown | D,P | No | Common recurrent secondary finding for t(8;21)[23][24]. |
Characteristic Chromosomal or Other Global Mutational Patterns
Additional chromosomal aberrations are infrequently seen in BCR-ABL AML, it has been described together with different class II aberrations such as CBFB-MYH11, RUNX1- RUNX1T1 and PML-RARA[25][5]. In AML, BCR-ABL1 seems to cooperate with several AML-specific aberrations such as inv(16), t(8;21) and myelodysplasia-related cytogenetic aberrations[5][25]. (For diagnostic purpose, note that inv(16) is not restricted to AML and can also be found in CML-MBC). Additional chromosomal aberrations, such as an additional Ph chromosome, trisomy 19 and isochromosome 17q seen in CML MBP are infrequently seen in AML with BCR::ABL1.
| Chromosomal Pattern | Molecular Pathogenesis | Prevalence -
Common >20%, Recurrent 5-20% or Rare <5% (Disease) |
Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | Established Clinical Significance Per Guidelines - Yes or No (Source) | Clinical Relevance Details/Other Notes |
|---|---|---|---|---|---|
| inv(16)(p13.1q22) or t(16;16)(p13.1;q22) | CBFB::MYH11 fusion | Rare (BCR-ABL1 AML) | D,P | No | The rarity of Philadelphia-positive subclones in AML patients with specific genetic lesions requires more cases for conclusive prognosis and therapeutic insights[25]. |
| t(8;21)(q22;q22.1) | RUNX1- RUNX1T1 | Rare (BCR-ABL1 AML) | D,P | No | The rarity of Philadelphia-positive subclones in AML patients with specific genetic lesions requires more cases for conclusive prognosis and therapeutic insights[25]. |
| t(15;17)(q13.4;q21.2) | PML-RARA | Rare (BCR-ABL1 AML) | D,P | No | The rarity of Philadelphia-positive subclones in AML patients with specific genetic lesions requires more cases for conclusive prognosis and therapeutic insights[25]. |
| AML-myelodysplasia-related (AML-MR) cytogenetic aberrations:
• del(5q), t(5q) • inv(3)(q21q26) • ‐7, del(7q) |
Unknown | Rare (BCR-ABL1 AML) | D,P | No | The rarity of Philadelphia-positive subclones in AML patients with specific genetic lesions requires more cases for conclusive prognosis and therapeutic insights[25].
In AML, BCR-ABL appears to interact with specific aberrations like inv(16) and myelodysplasia-related cytogenetic changes, like del(5q), t(5q)[25], inv(3)(q21q26)[25], ‐7, del(7q)[26], but the mechanisms of disease initiation and cooperation remain unclear[5]. |
Gene Mutations (SNV/INDEL)
RUNX1 mutation is common in AML with BCR::ABL1 and occurs in ~40% of cases[4]. Other mutated genes include ASXL1, BCOR, IDH1 / IDH2 and SRSF2; each of these occur in 10 - 15% of cases[27][28][4].Coinciding molecular events such as NPM1 mutations have been reported[25]. Mutations of FLT3 or DNMT3A are not commonly detected[4].
| Gene | Genetic Alteration | Tumor Suppressor Gene, Oncogene, Other | Prevalence -
Common >20%, Recurrent 5-20% or Rare <5% (Disease) |
Diagnostic, Prognostic, and Therapeutic Significance - D, P, T | Established Clinical Significance Per Guidelines - Yes or No (Source) | Clinical Relevance Details/Other Notes |
|---|---|---|---|---|---|---|
| RUNX1
|
Variable LOF and missense mutations | Tumor Suppressor Gene | Common (BCR-ABL1 AML) | D,P | No | AML with RUNX1 mutation is associated with a poorer prognosis[8]. RUNX1 was the most commonly mutated gene, altered in eight of 21 BCR-ABL1 AML cases (38%)[4].
Mutations in five genes (BCOR, BCORL1, SF3B1, SRSF2, and STAG2), along with ASXL1 and RUNX1 mutations, are linked to the proposed high-risk AML chromatin-spliceosome group[4]. |
| ASXL1 | Variable LOF and missense mutations | Tumor Suppressor Gene | Recurrent (BCR-ABL1 AML) | D,P | No | Mutations in five genes (BCOR, BCORL1, SF3B1, SRSF2, and STAG2), along with ASXL1 and RUNX1 mutations, are linked to the proposed high-risk AML chromatin-spliceosome group[4]. |
| BCOR | Variable LOF and missense mutations | Tumor Suppressor Gene | Recurrent (BCR-ABL1 AML) | D,P | No | Mutations in five genes (BCOR, BCORL1, SF3B1, SRSF2, and STAG2), along with ASXL1 and RUNX1 mutations, are linked to the proposed high-risk AML chromatin-spliceosome group[4]. |
| IDH1 / IDH2 | Missense | Oncogene | Recurrent (BCR-ABL1 AML) | D,P | No | Other mutated genes include ASXL1, BCOR, IDH1 / IDH2 and SRSF2; each of these occur in 10 - 15% of cases[27][28][4]. |
| SRSF2 | Missense and in frame del | Tumor Suppressor Gene | Recurrent (BCR-ABL1 AML) | D,P | No | Mutations in five genes (BCOR, BCORL1, SF3B1, SRSF2, and STAG2), along with ASXL1 and RUNX1 mutations, are linked to the proposed high-risk AML chromatin-spliceosome group[4]. |
| NPM1 | Variable LOF | Tumor Suppressor Gene and Oncogene | Rare (BCR-ABL1 AML) | D,P | No | Philadelphia-positive subclones can emerge in NPM1-mutated AML at diagnosis or during follow-up, and may cooperate with the NPM1 mutation like other class I mutations, such as FLT3-ITD or MLL-PTD[25]. |
Note: A more extensive list of mutations can be found in cBioportal, COSMIC, and/or other databases. When applicable, gene-specific pages within the CCGA site directly link to pertinent external content.
Epigenomic Alterations
Not applicable
Genes and Main Pathways Involved
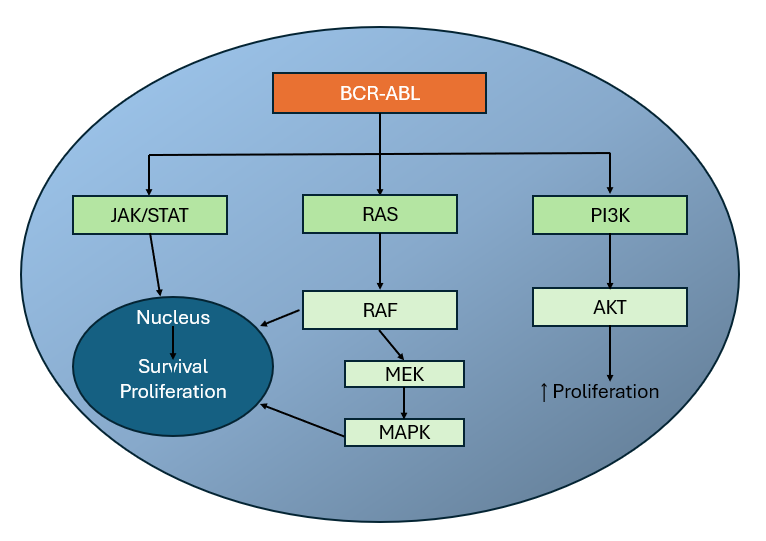
The BCR gene product has serine/threonine kinase activity and is a GTPase-activating protein for p21rac[29]. The ABL1 gene is a proto-oncogene that encodes a protein tyrosine kinase involved in a variety of cellular processes, including cell division, adhesion, differentiation, and response to stress. The activity of this protein is negatively regulated by its SH3 domain, whereby deletion of the region encoding this domain results in an oncogene[30]. The t(9,22)(q34;q11) leads to the formation of a Philadelphia chromosome and generates an active chimeric BCR-ABL1 tyrosine kinase. The fusion gene is created by juxtaposing the ABL1 gene on chromosome 9 (region q34) to a part of BCR (breakpoint cluster region) gene on chromosome 22 (region q11). This is a reciprocal translocation, creating an elongated chromosome 9 (der 9), and a truncated chromosome 22 (the Philadelphia chromosome, 22q-), the oncogenic BCR-ABL1 being found on the shorter derivative 22 chromosome[31][32]. This gene encodes for a BCR-ABL1 fusion protein, a tyrosine kinase. Tyrosine kinase activities are typically regulated in an auto-inhibitory manner, but the BCR-ABL1 fusion gene codes for a protein that is continuously activated, causing unregulated cell division. This is a result of the replacement of the myristoylated cap region which causes a conformational change rendering the kinase domain inactive, with a truncated portion of the BCR protein[33]. The enzyme is responsible for the uncontrolled growth of leukemic cells which survive better than normal blood cells. As a result of BCR/ABL1 variable splicing (fusion RNA and hybrid proteins), two transcripts p190 and p210 are found for BCR-ABL1 positive AML.
| Gene; Genetic Alteration | Pathway | Pathophysiologic Outcome |
|---|---|---|
| BCR and ABL1; Activating mutations | Ras/MAPK, PI3K/AKT, JAK/STAT and NF-kappaB pathways | The BCR-ABL fusion protein is an constitutively active tyrosine kinase that triggers multiple pathways, promoting unchecked cell proliferation and survival. |
Genetic Diagnostic Testing Methods
Bone marrow with myeloid blasts >20% combined with detection of t(9,22) by karyotype analysis or BCR-ABL1 using FISH or reverse transcriptase-quantitative PCR (RT-qPCR) and RNA or DNA seq[5]. A graphic of the clinical path for the differential diagnosis of BCR-ABL1 positive acute myeloid leukemia and chronic myeloid leukemia-myeloid blast crisis (CML-MBC) is presented[5].
Familial Forms
Not applicable
Additional Information
Not applicable
Links
Vogel A, et al. Acute Myeloid Leukemia with BCR-ABL1. SH2017-0299. Presentation at Society for Hematopathology / European Association for Haematopathology (SH/EAHP) 2017 Workshop. https://www.sh-eahp.org/images/2017_Workshop/3_3SH-EAHP%202017_AML%20with%20BCR-ABL1_%20AV%20FINAL.pdf (accessed 29th June 2018)
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Soupir, Chad P.; et al. (2007-04). "Philadelphia chromosome-positive acute myeloid leukemia: a rare aggressive leukemia with clinicopathologic features distinct from chronic myeloid leukemia in myeloid blast crisis". American Journal of Clinical Pathology. 127 (4): 642–650. doi:10.1309/B4NVER1AJJ84CTUU. ISSN 0002-9173. PMID 17369142. Check date values in:
|date=(help) - ↑ 2.0 2.1 2.2 Konoplev, Sergej; et al. (2013-01). "Molecular characterization of de novo Philadelphia chromosome-positive acute myeloid leukemia". Leukemia & Lymphoma. 54 (1): 138–144. doi:10.3109/10428194.2012.701739. ISSN 1029-2403. PMC 3925981. PMID 22691121. Check date values in:
|date=(help) - ↑ Nacheva, Ellie P.; et al. (2013-05). "Does BCR/ABL1 positive acute myeloid leukaemia exist?". British Journal of Haematology. 161 (4): 541–550. doi:10.1111/bjh.12301. ISSN 1365-2141. PMID 23521501. Check date values in:
|date=(help) - ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 Orsmark-Pietras, Christina; et al. (2021-06). "Clinical and genomic characterization of patients diagnosed with the provisional entity acute myeloid leukemia with BCR-ABL1, a Swedish population-based study". Genes, Chromosomes & Cancer. 60 (6): 426–433. doi:10.1002/gcc.22936. ISSN 1098-2264. PMID 33433047 Check
|pmid=value (help). Check date values in:|date=(help) - ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 Neuendorff, Nina Rosa; et al. (2016). "BCR-ABL-positive acute myeloid leukemia: a new entity? Analysis of clinical and molecular features". Annals of Hematology. 95 (8): 1211–1221. doi:10.1007/s00277-016-2721-z. ISSN 1432-0584. PMID 27297971.
- ↑ Arber DA, et al., (2017). Acute Myeloid Leukemia, in Hematopathology, 2nd Edition. Jaffe E, Arer DA, Campo E, Harris NL, and Quintanilla-Fend L, Editors. Elsevier:Philadelphia, PA, p817-846.
- ↑ Cuneo, A.; et al. (1996). "Philadelphia chromosome-positive acute myeloid leukemia: cytoimmunologic and cytogenetic features". Haematologica. 81 (5): 423–427. ISSN 0390-6078. PMID 8952155.
- ↑ 8.0 8.1 8.2 Pollyea DA, Altman JK, (2025). NCCN Clinical Practice Guidelines in Oncology: AML. Version 2. Available at: NCCN.org.
- ↑ Maiti, Abhishek; et al. (2020). "Venetoclax and BCR-ABL Tyrosine Kinase Inhibitor Combinations: Outcome in Patients with Philadelphia Chromosome-Positive Advanced Myeloid Leukemias". Acta Haematologica. 143 (6): 567–573. doi:10.1159/000506346. ISSN 1421-9662. PMC 7839068 Check
|pmc=value (help). PMID 32289808 Check|pmid=value (help). - ↑ Cross, Nicholas C. P.; et al. (2023-11). "European LeukemiaNet laboratory recommendations for the diagnosis and management of chronic myeloid leukemia". Leukemia. 37 (11): 2150–2167. doi:10.1038/s41375-023-02048-y. ISSN 1476-5551. PMC 10624636 Check
|pmc=value (help). PMID 37794101 Check|pmid=value (help). Check date values in:|date=(help) - ↑ Sawyers, C. L. (1999-04-29). "Chronic myeloid leukemia". The New England Journal of Medicine. 340 (17): 1330–1340. doi:10.1056/NEJM199904293401706. ISSN 0028-4793. PMID 10219069.
- ↑ Sharma, Diwakar; et al. (2024-08-01). "Does presence of complex translocations involving BCR::ABL1 in chronic myeloid leukemia affect the response rate to tyrosine kinase inhibitors? A systematic review of the literature". Annals of Diagnostic Pathology. 71: 152303. doi:10.1016/j.anndiagpath.2024.152303. ISSN 1092-9134.
- ↑ Cortes, Jorge E.; et al. (2003-05-15). "Prognostic significance of cytogenetic clonal evolution in patients with chronic myelogenous leukemia on imatinib mesylate therapy". Blood. 101 (10): 3794–3800. doi:10.1182/blood-2002-09-2790. ISSN 0006-4971. PMID 12560227.
- ↑ Branford, Susan; et al. (2014-07-24). "Prognosis for patients with CML and >10% BCR-ABL1 after 3 months of imatinib depends on the rate of BCR-ABL1 decline". Blood. 124 (4): 511–518. doi:10.1182/blood-2014-03-566323. ISSN 1528-0020. PMID 24859364.
- ↑ Lauseker, Michael; et al. (2023-11). "Survival with chronic myeloid leukaemia after failing milestones". Leukemia. 37 (11): 2231–2236. doi:10.1038/s41375-023-02028-2. ISSN 1476-5551. PMC 10624616 Check
|pmc=value (help). PMID 37726340 Check|pmid=value (help). Check date values in:|date=(help) - ↑ 16.0 16.1 Al Hamad, Mohammad (2021). "Contribution of BCR-ABL molecular variants and leukemic stem cells in response and resistance to tyrosine kinase inhibitors: a review". F1000Research. 10: 1288. doi:10.12688/f1000research.74570.2. ISSN 2046-1402. PMC 8886173 Check
|pmc=value (help). PMID 35284066 Check|pmid=value (help). - ↑ Tumours, 5th edition, IARC Press:Lyon, 2024. Online at: WHO Classification of Tumours.
- ↑ Shao, Xiaoyan; et al. (2018-11). "Primary Philadelphia chromosome positive acute myeloid leukemia: A case report". Medicine. 97 (44): e12949. doi:10.1097/MD.0000000000012949. ISSN 1536-5964. PMC 6221582. PMID 30383645. Check date values in:
|date=(help) - ↑ Lazarevic, Vladimir Lj; et al. (2018-01). "Relatively favorable outcome after allogeneic stem cell transplantation for BCR-ABL1-positive AML: A survey from the acute leukemia working party of the European Society for blood and marrow transplantation (EBMT)". American Journal of Hematology. 93 (1): 31–39. doi:10.1002/ajh.24928. ISSN 1096-8652. PMID 28971504. Check date values in:
|date=(help) - ↑ Konoplev, Sergej; et al. (2013-01). "Molecular characterization of de novo Philadelphia chromosome-positive acute myeloid leukemia". Leukemia & Lymphoma. 54 (1): 138–144. doi:10.3109/10428194.2012.701739. ISSN 1029-2403. PMC 3925981. PMID 22691121. Check date values in:
|date=(help) - ↑ Nacheva, Ellie P.; et al. (2013). "Does BCR/ABL1 positive acute myeloid leukaemia exist?". British Journal of Haematology. 161 (4): 541–550. doi:10.1111/bjh.12301. ISSN 1365-2141. PMID 23521501.
- ↑ Arber DA, et al., (2017). Acute myeloid leukaemia with recurrent genetic abnormalities, in World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues, Revised 4th edition. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Arber DA, Hasserjian RP, Le Beau MM, Orazi A, and Siebert R, Editors. Revised 4th Edition. IARC Press: Lyon, France, p140.
- ↑ Jakovic, Ljubomir; et al. (2022-09-01). "De novo acute myeloid leukemia harboring concomitant t(8;21)(q22;q22);RUNX1::RUNX1T1 and BCR::ABL1 (p190 minor transcript)". Journal of Hematopathology. 15 (3): 191–195. doi:10.1007/s12308-022-00509-4. ISSN 1865-5785.
- ↑ Singh, Manish K.; et al. (2017-03-01). "Co-existence of AML1-ETO and BCR-ABL1 transcripts in a relapsed patient of acute myeloid leukemia with favorable risk group: A coincidence or clonal evolution?". Hematology/Oncology and Stem Cell Therapy. 10 (1): 39–41. doi:10.1016/j.hemonc.2015.12.003. ISSN 1658-3876.
- ↑ 25.00 25.01 25.02 25.03 25.04 25.05 25.06 25.07 25.08 25.09 Bacher, Ulrike; et al. (2011). "Subclones with the t(9;22)/BCR-ABL1 rearrangement occur in AML and seem to cooperate with distinct genetic alterations". British Journal of Haematology. 152 (6): 713–720. doi:10.1111/j.1365-2141.2010.08472.x. ISSN 1365-2141. PMID 21275954.
- ↑ Tirado, Carlos A.; et al. (2010-07). "Acute myeloid leukemia with inv(16) with CBFB–MYH11, 3′CBFB deletion, variant t(9;22) with BCR–ABL1, and del(7)(q22q32) in a pediatric patient: case report and literature review". Cancer Genetics and Cytogenetics. 200 (1): 54–59. doi:10.1016/j.cancergencyto.2010.03.001. ISSN 0165-4608. Check date values in:
|date=(help) - ↑ 27.0 27.1 Konoplev, Sergej; et al. (2013-01). "Molecular characterization of de novo Philadelphia chromosome-positive acute myeloid leukemia". Leukemia & Lymphoma. 54 (1): 138–144. doi:10.3109/10428194.2012.701739. ISSN 1029-2403. PMC 3925981. PMID 22691121. Check date values in:
|date=(help) - ↑ 28.0 28.1 Eisfeld, A.-K.; et al. (2017-10). "The mutational oncoprint of recurrent cytogenetic abnormalities in adult patients with de novo acute myeloid leukemia". Leukemia. 31 (10): 2211–2218. doi:10.1038/leu.2017.86. ISSN 1476-5551. PMC 5628133. PMID 28321123. Check date values in:
|date=(help) - ↑ Maru, Y.; et al. (1991). "The BCR gene encodes a novel serine/threonine kinase activity within a single exon". Cell. 67 (3): 459–468. doi:10.1016/0092-8674(91)90521-y. ISSN 0092-8674. PMID 1657398.
- ↑ Wang, Jean Y. J. (2014). "The capable ABL: what is its biological function?". Molecular and Cellular Biology. 34 (7): 1188–1197. doi:10.1128/MCB.01454-13. ISSN 1098-5549. PMC 3993570. PMID 24421390.
- ↑ Kurzrock, Razelle; et al. (2003). "Philadelphia chromosome-positive leukemias: from basic mechanisms to molecular therapeutics". Annals of Internal Medicine. 138 (10): 819–830. doi:10.7326/0003-4819-138-10-200305200-00010. ISSN 1539-3704. PMID 12755554.
- ↑ Melo, J. V. (1996). "The diversity of BCR-ABL fusion proteins and their relationship to leukemia phenotype". Blood. 88 (7): 2375–2384. ISSN 0006-4971. PMID 8839828.
- ↑ Nagar, Bhushan; et al. (2003). "Structural basis for the autoinhibition of c-Abl tyrosine kinase". Cell. 112 (6): 859–871. doi:10.1016/s0092-8674(03)00194-6. ISSN 0092-8674. PMID 12654251.
Notes
*Primary authors will typically be those that initially create and complete the content of a page. If a subsequent user modifies the content and feels the effort put forth is of high enough significance to warrant listing in the authorship section, please contact the Associate Editor or other CCGA representative. When pages have a major update, the new author will be acknowledged at the beginning of the page, and those who contributed previously will be acknowledged below as a prior author.
Prior Author(s):
Kay Weng Choy MBBS, Monash Medical Centre
*Citation of this Page: “Acute myeloid leukaemia with BCR::ABL1 fusion”. Compendium of Cancer Genome Aberrations (CCGA), Cancer Genomics Consortium (CGC), updated 07/3/2025, https://ccga.io/index.php/HAEM5:Acute_myeloid_leukaemia_with_BCR::ABL1_fusion.